More Information
Submitted: May 22, 2025 | Approved: June 03, 2025 | Published: June 04, 2025
How to cite this article: Deshmukh Mahesh K, Galani Komal S, Manisha M, Pooja I. Pulmonary Pleomorphic Carcinoma: A Rare Entity Revisited!. J Pulmonol Respir Res. 2025; 9(1): 023-025. Available from:
https://dx.doi.org/10.29328/journal.jprr.1001069
DOI: 10.29328/journal.jprr.1001069
Copyright license: © 2025 Deshmukh Mahesh K, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: EGFR; Pulomonary pleomorphic carcinoma; Surgical resection
Pulmonary Pleomorphic Carcinoma: A Rare Entity Revisited!
Deshmukh Mahesh K1, Galani Komal S2*, Mishra Manisha3 and Ingale Pooja3
1Consultant Pathologist, Alexis Multispeciality Hospital, India
2Consultant Pathologist, Star Superspeciality Hospital, India
3Consultant Pathologist, RST Cancer Hospital, India
*Address for Correspondence: Niroshan Ranjan, MD, Henry Ford Allegiance Hospital, 1909 Apt 1 Springport Rd, Jackson, MI, 49202, USA, Email: [email protected]
Introduction: Pleomorphic Carcinoma (PC) is a subset of poorly differentiated non–small cell lung cancer that is diagnostically challenging because it is a rare malignancy of the lung. It shows varying dual-cell components; spindle or giant cells and epithelial cells.
Method: We report a case of 68-year-old non-smoking female who presented with cough, fever, pain in the left side of chest & weight loss of recent onset and an abnormal shadow on her chest X-ray. Computed tomography of chest revealed a well defined heterogeneously enhancing cavitatory soft tissue lesion in the posterior basal segment of the left lower lobe with mediastinal lymphadenopathy.
Results: Fine needle aspiration cytology& percutaneous lung biopsy confirmed poorly differentiated malignant tumor. Patient underwent a left lower lobectomy. A diagnosis of PC was confirmed after Immunohistochemistry (IHC). Mutation analysis revealed an EGFR exon 21 mutation within the tumor cells. The patient is on Gefitinib based chemotherapy and has remained disease-free for three years post-surgery.
Conclusion: PC of the lung is a rare pathological entity. Definite diagnosis may only be made on a resected tumor along with the use of IHC. Surgical resection is the main modality of the treatment. Such rare cases should be documented to establish an optimal management plan and to provide a further insight to targeted therapy.
Pulmonary Pleomorphic Carcinoma (PC) is a rare malignant tumor of the lung and its incidence has been reported to range from 0.1% to 0.4% of all lung cancer [1]. According to the newer WHO classification, PC is a poorly differentiated non-small cell carcinoma that contains at least 10% spindle and /or giant cells [2]. Definite diagnosis may only be made on a resected tumor. It has a more aggressive clinical course and a worse outcome than other Non-Small Cell Lung Cancer (NSCLC) [3]. Identification of this tumor requires knowledge of specific histologic criteria & immunohistochemical studies alongwith correlation with chest imaging. In the present study, we report such an extremely rare case.
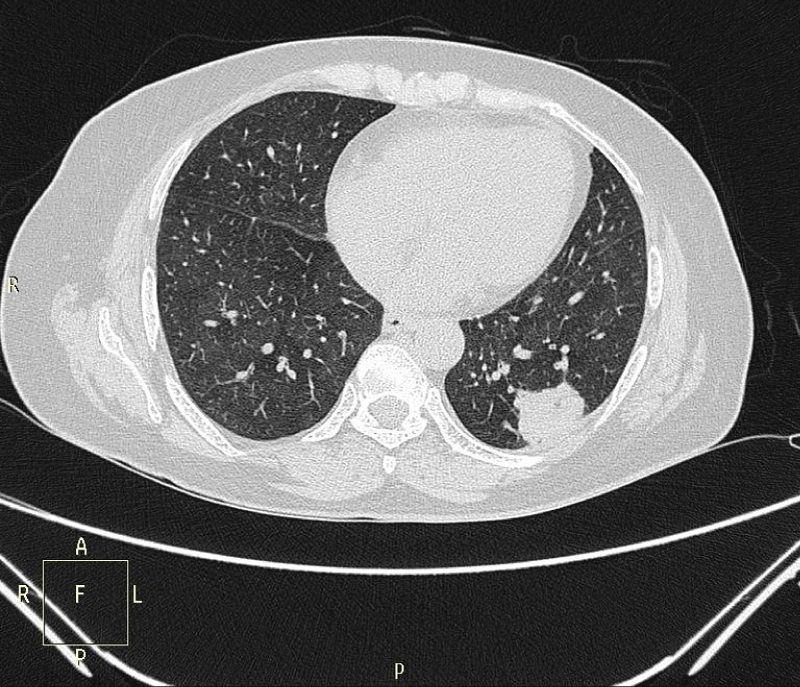
A 68-year-old female non-smoker, initially presented with cough & fever followed by significant weight loss (8 kgs in 2 months), loss of appetite & pain in the left side of chest of two months duration. There was no prior history of any lung disease. Chest X-ray revealed an abnormal patch in the left lower lobe of the lung. Computed Tomography (CT) of chest revealed a well defined heterogeneously enhancing cavitatory soft tissue lesion with spiculated margin in the posterior basal segment of the left lower lobe (Figure 1). The lesion was attached to the posterior chest wall with mediastinal lymphadenopathy. Lymph node staging was not done as whole body PET CT scan showed no obvious evidence of any distant metastasis.
Figure 1: Computed tomography scan of the chest shows a solid tumor in the left lung lobe.
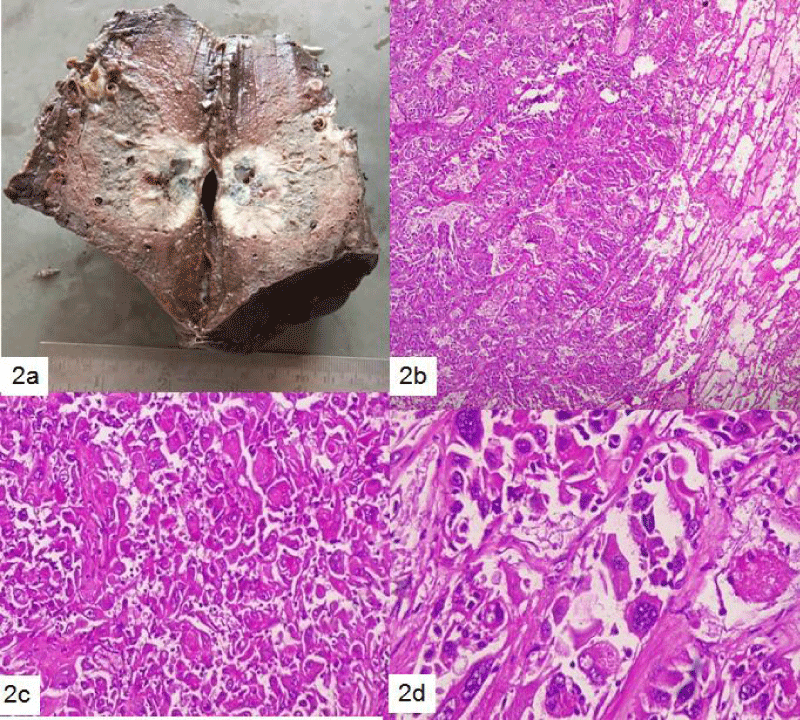
CT guided Fine needle aspiration cytology & biopsy from the mass showed malignant cells in sheets & clusters showing high pleomorphism, hyperchromatic nuclei with abundant cytoplasm. Numerous mitotic figures were seen. Patient underwent a left lower lobectomy. Grossly, a firm grey-white solid-cystic peripheral tumor measuring 4.1 × 3 × 2 cm was seen in the left lower lobe with pleura adherent to the tumor (Figure 2). Histological examination revealed poorly differentiated tumor cells (~80%) with hyperchromatic nuclei and multinucleated giant cells (~20%).
Figure 2: (a): Gross features of the tumor. The tumor is grey-white, firm with necrotic foci and reaches upto the pleura, (b): The tumor consists of malignant spindle cells, polygonal cells and giant cells (Hematoxylin & eosin, 40x), (c) Pleomorphic tumor cells (100x) and (d) malignant spindle cells with bizarre nuclei (400x).
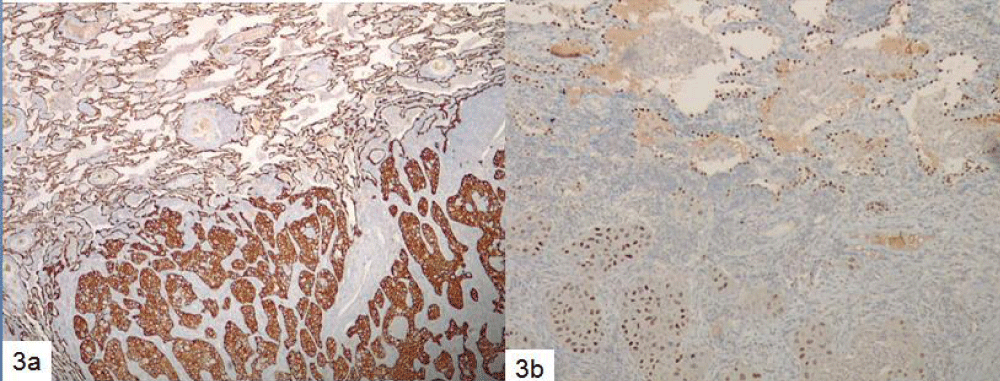
Areas of necrosis were also noted. In addition, the dissected mediastinal lymph nodes were free of tumor. On immunohistochemical evaluation, the tumor cells expressed cytokeratin-7 and thyroid transcription factor (TTF-1), but were negative for p40 and Anaplastic Lymphoma Kinase (ALK) protein (Figure 3). Finally, a diagnosis of Pulmonary Pleomorphic carcinoma was rendered (pathological stage T2aN0M0).
Figure 3: Immunostaining: (a): Cytokeratin-7 diffuse staining highlights tumor cells and adjacent pneumocytes (40x). (b) Thyroid transcription factor -1 positivity seen as nuclear staining (40x).
The tumor cells were found to be EGFR exon 21 mutated by real-time Polymerase Chain Reaction (PCR) while no ROS1 gene rearrangement was detected by Fluorescence in situ Hybridization (FISH). Patient was offered surgical treatment followed by targeted treatment as Chemotherapy is of limited efficacy. The patient is on Gefitinib-based chemotherapy and has remained cancer-free during three years of annual follow-up visits after surgery, without any major complaints.
Carcinomas comprising a mixture of spindle and giant cell component qualify as Pleomorphic carcinoma. The incidence of PC ranges from 0.1% to 0.4% of all lung cancers, with only a few case reports published to date. Common presenting symptoms include cough, hemoptysis, chest pain, and fever. Mean age at diagnosis is 60 to 65 years with a male preponderance (male: female ratio of 2.1:1). There is a strong correlation with smoking as shown in 60% - 90% of Ex-smokers who developed PC [1,4]. Due to the extreme rarity of these cases, the exact incidence in different ethnic groups is not reported. Our patient in this study was an elderly female with recent onset respiratory symptoms.
On CT scan, most lesions present as peripheral large masses & cavity lesions, like the index case, with substantial enhancement and often showing signs of myxoid degeneration, hemorrhage and necrosis. Diagnosis of PC relies heavily on resected surgical specimens because of its biphasic appearance and its frequent association with other histological types. In PC, the giant and/or spindle elements, comprising at least 10% of the tumor, are admixed with components such as adenocarcinoma (31% - 72%), squamous cell carcinoma (12% - 26%) or undifferentiated non small cell carcinoma (in up to 43% of cases) [2]. In the present case, adenocarcinoma was admixed with pleomorphic component. Due to limited biopsy material, PC may be misdiagnosed unless seen in the resected specimen. Conventional carcinoma and sarcoma components in these tumors are often inconspicuous & display striking morphologic variability. With a Therefore, in resection specimens, adequate sampling is essential and should include at least one section per centimeter of maximum tumor diameter.
Several antibodies used to evaluate the pulmonary & epithelial nature of this tumor include thyroid transcription factor-1, surfactant apoprotein-A, and cytokeratins while vimentin is expressed in the sarcomatous elements. We also performed ALK protein which was negative in our case.
PC exhibits an aggressive clinical course characterized by rapid growth, invasion of adjacent structures, and early metastasis. PC shows a worse outcome due to high relapse rate. More aggressive treatment strategy is warranted. There are no defined guidelines on the treatment of PC. PCs are difficult to treat. Surgery provides the best chance for survival whereas palliative chemotherapy is advised in advanced cases. Conventional radiation therapy has had little effect on PC. For patients with mutated Epidermal Growth Factor Receptor (EGFR), targeted therapy with Tyrosine Kinase Receptor Inhibitors (TKIs) is an option that most likely helps in achieving disease regression and survival benefit. In the study by Kiara, et al. [4], of small sample size (n = 17), the incidence of EGFR mutation was approximately 20%, and EGFR mutations were observed in patients with a carcinomatous element of adenocarcinoma like in our patient. The likely homogeneity of tumor cells in terms of EGFR mutation status may have contributed to the observed response to the response to Gefitinib for 3 years. Nevertheless, careful management is warranted due to the limited duration of benefit from EGFR-TKIs in patients with EGFR-mutant tumors [4,5]. In the study by Jia X, EGFR mutations were commonly identified in women; Therefore, female patients should be prioritized for EGFR mutation screening as in our index case [6,7].
Favorable prognostic factors reported include complete surgical resection, no lymph nodes metastasis, lower pathologic stages, and tumor necrosis. Pleural involvement has been identified as an adverse prognostic factor. Overall, the prognosis for PC is poor. Fishback, et al. and Rossi, et al. reported the median survival time is 8 to 19 months [4,5]. Chang, et al. [1] reported that 7 patients who received surgical resections has distal metastases within a few months [1]. Chang, et al. [1] also reported the median survival time was only 3 months for 9 inoperable cases that were treated by chemoradiotherapy. In our case, the patient underwent complete resection and the pathological stage was T2aN0M0 (Stage Ib). The patient is on Gefitinib based chemotherapy and has been living cancer-free since three years after the surgery without any major complaints. Tumor biology needs to be explored further to understand such a course of the disease.
Pleomorphic carcinoma is a rare aggressive lung tumor with a very low incidence. Clinicians should consider the possibility of this tumor in rapid-growing and early-disseminating tumors. Awareness about this entity & its heterogenous morphology helps in early diagnosis. Though it carries a poorer prognosis as compared to other non-small cell lung cancers, targeted treatment is available. Also, female patients should be prioritized for EGFR mutation screening. Documenting such cases would help understand the biology of this tumor & establish appropriate treatment methods.
The authors thank Dr P Joshi (MS), Senior Consultant from Department of Surgery, RST Cancer Center and Dr. Maj. Prashant Nimbalkar (MD, DNB Radiodiagnosis) for their timely support.
- Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer 2001; 34: 91–97. Available from: https://doi.org/10.1111/j.1348-0421.2008.00083.x
- Kerr KM, Pelosi G, Austin JHM. World Health Organization Classification of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press; 2017:88–90.
- Rossi G, Cavazza A, Sturm N, Migaldi M, Facciolongo N, Longo L, Maiorana A, Brambilla E. Pulmonary carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements: a clinicopathologic and immunohistochemical study of 75 cases. Am J Surg Pathol. 2003;27(3):311-24. Available from: https://doi.org/10.1097/00000478-200303000-00004
- Kaira K, Horie Y, Ayabe E, Murakami H, Takahashi T, Tsuya A, Nakamura Y, Naito T, Endo M, Kondo H, Nakajima T, Yamamoto N. Pulmonary pleomorphic carcinoma: a clinicopathological study including EGFR mutation analysis. J Thorac Oncol. 2010;5(4):460-5. Available from: https://doi.org/10.1097/jto.0b013e3181ce3e3c
- Zhang X, Wang Y, Zhao L, Jing H, Sang S, Du J. Pulmonary pleomorphic carcinoma: A case report and review of the literature. Medicine (Baltimore). 2017;96(29):e7465. Available from: https://doi.org/10.1097/md.0000000000007465
- Kawamura A, Tanaka Y, Inoue Y, Tsuchida T, Katsumata M, Karayama M, et al. EGFR-mutated, metastatic pulmonary pleomorphic carcinoma successfully treated with afatinib, Current Problems in Cancer: Case Reports. 2022:6:100160. Available from: https://doi.org/10.1016/j.cpccr.2022.100160
- Jia X, Chen G. EGFR and KRAS mutations in pulmonary pleomorphic carcinoma and their correlation with clinicopathologic features. Contemp Oncol (Pozn). 2015;19(1):22-7. Available from: https://doi.org/10.5114/wo.2014.43491