More Information
Submitted: January 03, 2022 | Approved: January 27, 2022 | Published: January 28, 2022
How to cite this article: Sergio PG, Elena Y, María RJS, Nuria GG, Edwin MN. Spontaneous pneumomediastinum: case report. J Pulmonol Respir Res. 2022; 6: 001-003.
DOI: 10.29328/journal.jprr.1001034
Copyright License: © 2022 Sergio PG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Spontaneous pneumomediastinum; Asthma; Subcutaneous emphysema
Spontaneous pneumomediastinum: case report
Pedrós García Sergio1, Yakasova Elena2, Roquet-Jalmar Saus María3, Gutiérrez González Nuria2 and Mercedes Noboa Edwin2*
1Anesthesiology Department, Hospital Virgen de la Luz de Cuenca, Spain
2Pulmonology Department, Hospital Virgen de la Luz de Cuenca, Spain
3Radiology Department, Hospital Virgen de la Luz de Cuenca, Spain
*Address for Correspondence: Dr. Mercedes Noboa Edwin, Pulmonology Department, Virgen de la Luz Hospital, Hermandad de Donantes de Sangre, 1, 16002 Cuenca, Spain, Email: [email protected]
Pneumomediastinum is the presence of free air within the mediastinum. As a general rule, it occurs in the presence of underlying lung disease and if it does not exist, it is called spontaneous pneumomediastinum. We present a case of a 53 years old asthmatic patient which further investigation revealed to be consistent with spontaneous pneumomediastinum. He underwent medical treatment with relative rest, oxygen therapy, and prophylactic antibiotic therapy, in addition to his usual asthma treatment. There was a clinical and radiological improvement with complete passive reabsorption of air and the patient was discharged on the 4th day and referred to the pulmonology department for consultation. During 2 months follow-up period, there were no signs of recurrence.
Pneumomediastinum is the presence of air or gas in the mediastinum. It usually occurs in the presence of underlying lung disease such as asthma or chronic obstructive pulmonary disease (COPD) or it is related to precipitating factors such as trauma, invasive procedures (cervical, thoracic or abdominal), tracheobronchial or bronchoesophageal fistulas, Valsalva maneuver, positive-pressure mechanical ventilation, cough, vomiting, physical exercise or use of inhaled drugs, among others [1,2]. If one of these is not present, it is called spontaneous pneumomediastinum (SP). It is a rare entity and usually occurs in young adults, being more frequent in men [3]. Of the total number of patients admitted for SP, approximately 1% have a history of bronchial asthma [4].
We present a case of SP with subcutaneous emphysema in a man with a history of severe asthma who presented to the emergency room with cervical tightness, odynophagia, and changes in his tone of voice.
*We hope that this case provides ideas for clinicians to deal with the diagnosis of diseases with dysphagia as the main complaint and include the differential diagnosis of spontaneous pneumomediastinum*.
A 53-year-old man ex-smoker of 10 packs-year who presented to the emergency room with a 4- day history of odynophagia, slight edema in the oropharyngeal area, and the appearance, in the last 24 hours, of cervical oppression and changes in tone of his voice. He denied dyspnea or chest pain,
*prior to the onset of symptoms, had no triggers such as cough, vomiting, or chest trauma.
*His medical history included nasal polyposis, pansinusitis, and severe eosinophilic asthma well controlled. His therapy consisted of beclomethasone/formoterol, tiotropium, and montelukast as well as mepolizumab since July 2019. Had no other personal or family history of interest.
On physical examination, he was alert and oriented with a Glasgow score of 15/15. His respiratory rate was 16 breaths per minute, was not distressed. Cardiopulmonary auscultation was normal. Examination of the chest revealed crepitations on palpation consistent with extensive subcutaneous emphysema in the cervical and upper thoracic area. The remainder of the physical examination was unremarkable. Vital signs revealed blood oxygen saturation was 93% on room air, the pulse was 84 beats per minute, and blood pressure of 119/72 mmHg. Capillary blood glucose was 84 mg/dL and temperature 97.2 ºF (36.2 ºC).
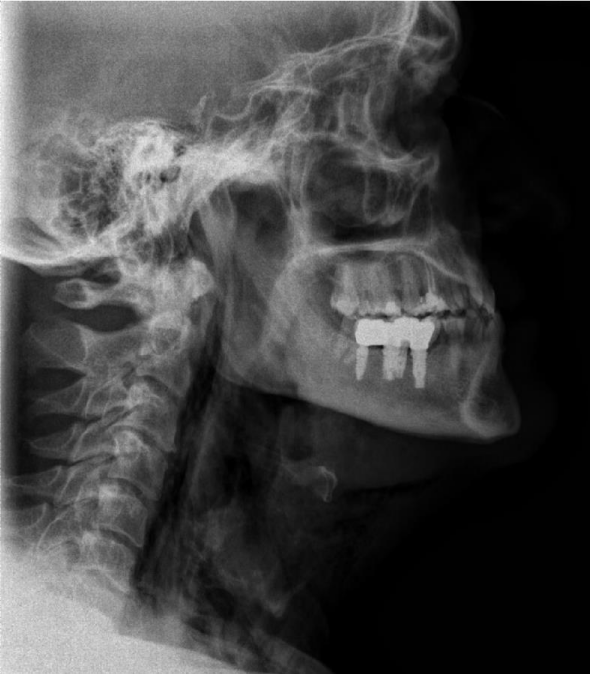
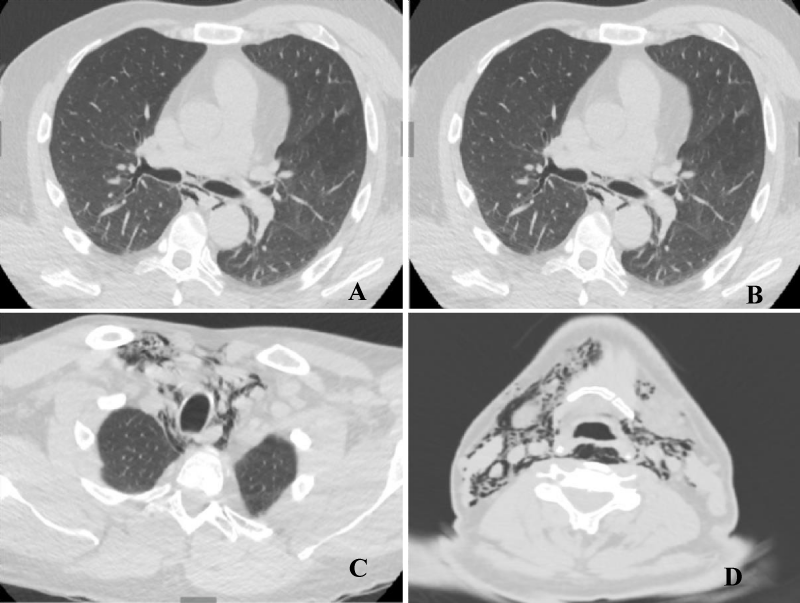
A chest X-ray (Figure 1) showed extensive subcutaneous emphysema at the cervical level and a chest computed tomography (CT) was requested, confirming the presence of pneumomediastinum and subcutaneous emphysema without finding any apparent valuable etiology also without evidence of free fluid and alterations at tracheal or esophageal level (Figure 2). Laboratory workup only revealed the presence of 14.300/mmc leukocytes with normal leukocyte formula and C-reactive protein 1.8 mg/L. The diagnosis of SP was established, during his hospitalization the patient received treatment with relative rest, oxygen therapy, and prophylactic antibiotic therapy, in addition to his usual treatment for bronchial asthma, presenting a favorable clinical and radiological evolution.
Figure 1: Cervical radiography lateral projection: subcutaneous emphysema that ascends to the cervical region.
Figure 2: Computed tomography. A: axial slice in lung window, shows air in the middle mediastinum surrounding main bronchi, esophagus, and hemiacigus vein. B: coronal slice in lung window, where pneumomediastinum is observed without pneumothorax. Emphysema of the soft tissues of the upper mediastinum and neck with aerial dissection of the muscular and vascular structures (C and D).
He was discharged on the 4th day and a scheduled revision was proposed at 2 weeks and at the second month in the pneumology consultation. During the follow-up, there were no data on the recurrence of pneumomediastinum, and from the point of view of bronchial asthma, it remained well controlled with its usual treatment without requiring modifications of it.
Spontaneous pneumomediastinum is a rare entity that usually occurs in young adults, with a male/female ratio of 8:13, and is usually associated with a pre-existing respiratory disease such as asthma or COPD. Our case shares several of these aspects, however, the age of presentation of our patient exceeds 50 years, an unusual fact in the cases published to date in the literature, where the age generally ranges from 18 to 30 years [5].
In the publication of Alemu, et al. a bibliographic search was made for patients with spontaneous pneumomediastinum, finding a total of 339 cases published. As of 1960, there were only 4 (1.2%) cases reported and by 2000 the number published in the literature reached 76 (22.4%). Since then, 259 (76.4%) cases have been published. Most reports came from Asia (176 [51.9%]) followed by the United States of America (95 [28%]), Europe (53 [15.6%]), Canada (6 [1.8%]), South America (4 [1.2%]), Africa (3 [0.88%]) and Australia (2 [0.5%]) [3]. More than 80% of cases are concentrated in Asia, the United States, and Canada, with only 54 cases reported to date across Europe, including ours.
Physiopathologically, the trigger factor in spontaneous pneumomediastinum is the rupture of the terminal alveoli due to an increase in intra-alveolar pressure and, consequently, to air leakage in the pulmonary interstitium and from there to the pulmonary helium and the mediastinum. Air in the mediastinum can pass through the fascia and spread to subcutaneous tissue in the chest and cervical region, retropharyngeal space, peritoneum, retroperitoneum, and pericardium. This mechanism was described and demonstrated by Macklin in 1944 [6,7].
The most common form of presentation of spontaneous pneumomediastinum is chest pain and dyspnea. Other symptoms are cough, nasal voice, cervical pain, dysphonia, swelling, and dysphagia. A large series of cases published by Campillo, et al. reported 36 patients in whom chest pain and dyspnea were the most frequent presenting symptoms [8].
More than half of the cases (21) had lung diseases among their history, with asthma and COPD being the most common pathologies with 14 and 7 cases, respectively. Although the association between spontaneous pneumomediastinum and asthma is very frequent, its appearance is independent of the degree of control of this lung disease. In our case, the patient was in optimal control of his respiratory pathology.
With regards to physical examination, the most notable finding is the presence of subcutaneous emphysema, which is usually distributed from the shoulders to the neck. Some authors describe subcutaneous emphysema as a benign clinical sign because the air outlet between subcutaneous tissues prevents increased pressure within the mediastinum and compression of the larger vessels. Hamman’s sign is known as a sign in auscultation in spontaneous pneumomediastinum, which is identified in about 30% of patients and consists of the presence of crunching and bubbling sounds coinciding with the heartbeats [5].
Among the diagnostic tests, a chest X-ray is of choice, however, the posteroanterior projection establishes the diagnosis in half of the cases, which makes it important to obtain a lateral projection that allows the diagnosis in 100% of the cases [9]. Chest CT provides clarity in cases where the X-ray is inconclusive, as well as determining the degree of the extent and ruling out other associated lesions. In the case described, a chest CT scan was requested to rule out the presence of tracheal rupture, given the patient’s history of bronchial asthma. As no associated lesions were found at the trachea or oesophageal level and the short extension of the pneumomediastinum seen on chest CT, no further complementary tests were requested, according to similar published cases.
The differential diagnosis of spontaneous pneumo-mediastinum includes serious diseases such as primary pneumothorax, pericarditis, pulmonary embolism, acute coronary syndromes, Boerhaave syndrome, among others [5]. In our case, none of these was demonstrated. The presence of a foreign body in the esophagus should also be included in the differential diagnosis for odynophagia as a presenting symptom. This was reasonably ruled out with the absence of digestive history and normal chest CT.
Treatment is basically supportive, with analgesia, rest, avoiding maneuvers that increase chest pressure, etc. In general, no special interventions are indicated, provided there are no complications that require additional measures. High concentration oxygen therapy is explained by the fact that it reduces the partial pressure of nitrogen in the capillaries, thereby increasing the rate of reabsorption of the gas contained in the pleural space. Most cases have a favorable course with complete absorption of the air [10]. Other measures such as prophylactic use of antibiotics are not necessary if there are no severe symptoms or significant signs of inflammation. As a general rule, the course is satisfactory with conservative treatment, although, in exceptional cases, they may require mediastinotomy when it is so severe that it causes high intrathoracic tension. This is much rarer and limited to patients with post-traumatic pneumomediastinum and undergoing mechanical ventilation.
In summary, the symptomatology and evolution of the case presented was typical, with resolution within a few days of admission and absence of recurrence during subsequent follow-up in consultation. The association between spontaneous pneumomediastinum and asthma is very common, and odynophagia as a presentation implies including digestive pathologies such as the presence of a foreign body in the esophagus, among others, in the differential diagnosis.
- Ojha S, Gaskin J. Spontaneous pneumomediastinum. Bristol, UK. BMJ Case Rep. 2018.
- Semedo FHMA, Silva RS, Pereira S, Alfaiate T, Costa T, et al. Spontaneous pneumomediastinum: case report. Rev Assoc Med Bras. 2012; 58: 355-357. PubMed: https://pubmed.ncbi.nlm.nih.gov/22735229/
- Alemu B, Yeheyis ET, Tiruneh AG. Spontaneous primary pneumomediastinum: is it always benign? J Med Case Rep. 2021; 15: 157. PubMed: https://pubmed.ncbi.nlm.nih.gov/33761988/
- Ryoo JY. Clinical analysis of spontaneous pneumomediastinum. Tuberc Respir Dis. 2012; 73: 169-173. PubMed: https://pubmed.ncbi.nlm.nih.gov/23166550/
- Takada K, Matsumoto S, Hiramatsu T, Kojima K, Shizu M, et al. Spontaneous pneumomediastinum: an algorithm for diagnosis and management. Ther Adv Respir Dis. 2009; 3: 301-307. PubMed: https://pubmed.ncbi.nlm.nih.gov/19934282/
- Song Y, Lingfang Tu, Jianyong Wu. Pneumorrhachis with spontaneous pneumomediastinum and subcutaneous emphysema. Intern Med. 2009; 48: 1713-1714.
- Romero Kleber J, Trujillo Máximo H. Spontaneous pneumomediastinum and subcutaneous emphysema in asthma exacerbation: The Macklin effect. Heart Lung. 2010; 39: 444-447.
- Campillo A, Coll-Salinas A, Soria-Aledo V, Blanco-Barrio A, Flores-Pastor B, et al. Spontaneous Pneumomediastinum: Descriptive Study of Our Experience With 36 Cases. Arch Bronconeumol. 2005; 41: 528-531. PubMed: https://pubmed.ncbi.nlm.nih.gov/16194517/
- Lopes F. Pneumomediastino espontâneo após esforço vocal: relato de caso. Radiol Bras. 2010; 43: 137-139.
- Rodríguez M. Neumomediastino espontáneo tras esfuerzos tusígenos. Revista portuguesa de otorrinolaringologia e cirurgia cérvico-facial. 2014; 52: 183-186.