More Information
Submitted: January 17, 2024 | Approved: January 29, 2024 | Published: January 30, 2024
How to cite this article: Klepikov I. The Importance of The Concept of Acute Pneumonia for Choosing the Principles of its Treatment and Results. J Pulmonol Respir Res. 2024; 8: 003-008. .
DOI: 10.29328/journal.jprr.1001051
Copyright License: © 2024 Klepikov I. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The Importance of The Concept of Acute Pneumonia for Choosing the Principles of its Treatment and Results
Igor Klepikov*
Pediatric Surgeon, Renton, Washington, USA
*Address for Correspondence: Igor Klepikov, MD, Professor, Retired, Pediatric Surgeon, Renton, Washington, USA, Email: [email protected]
Over the past many decades, scientific research and practical efforts in the field of acute nonspecific inflammation of the lung tissue have been aimed at early detection of the pathogen and its suppression. Such a bacteriological diagnosis was always accompanied by doubts about its reliability and the results of treatment continued to slowly but steadily decrease. The following materials, which were received several decades ago and remained at the disposal of the author of these studies, have already been repeatedly published in the open press when discussing various aspects of the problem raised and remain available to interested readers. However, in this context, the most informative information and illustrations are summarized in order to present the information in an abbreviated version, which allows us to see and evaluate the fundamental role and importance of the disease concept for substantiating therapeutic principles and obtaining final results.
Acute Pneumonia (AP) is one of the oldest nosologies known to medicine throughout its foreseeable history. With such a long chronology, the treatment of this category of patients for most of this period did not have a scientifically based concept of the disease and was carried out using empirically selected methods. Despite the lack of a convincing theoretical basis, such therapy has enjoyed a certain popularity and relevance for many centuries, which is indirect evidence of its positive qualities. Currently, when scientific ideas about lung tissue inflammation have been significantly enriched, and modern medicine is failing in the treatment of the most severe category of these patients, data on the correction of the disease concept and the results of clinical trials of modified therapeutic principles may be of interest to specialists in this field.
Drastic changes in the state of this branch of medicine began to occur from the moment of the release and use of antibiotics. The selective antimicrobial effect of these drugs was known even before their clinical use, but the first results of such therapy created a false fascinating effect by the simplicity of their achievement, which made it possible to consider the causative agent of the process as the main cause of inflammatory nonspecific diseases. Another paradox on which subsequent generations of doctors were brought up was, on the one hand, the gradual and steady decrease in the activity of antibiotics, the spread of resistant strains, and unprecedented changes in the list of pathogens of AP. On the other hand, despite the expansion of our knowledge and ideas in the field of lung physiology and pathophysiology, active efforts were made to preserve the leading therapeutic role of antimicrobials, the fanatical nature of which was reflected in their inconsistency with new facts of reality.
The continuous decrease in the effectiveness of antibacterial therapy increasingly began to require the use of additional care products, the choice of which was determined by the leading role of the pathogen of AP and did not take into account the specifics of its pathogenesis. As a result of this concept, procedures from the general therapeutic set, which contradicted the basics of the pathogenesis of the disease, began to be used as a means of additional assistance. Infusion therapy turned out to be one of such widely demanded methods, and the typical dynamics of the process in such situations attracted our attention more than forty years ago, as demonstrated by an example of one of the past observations.
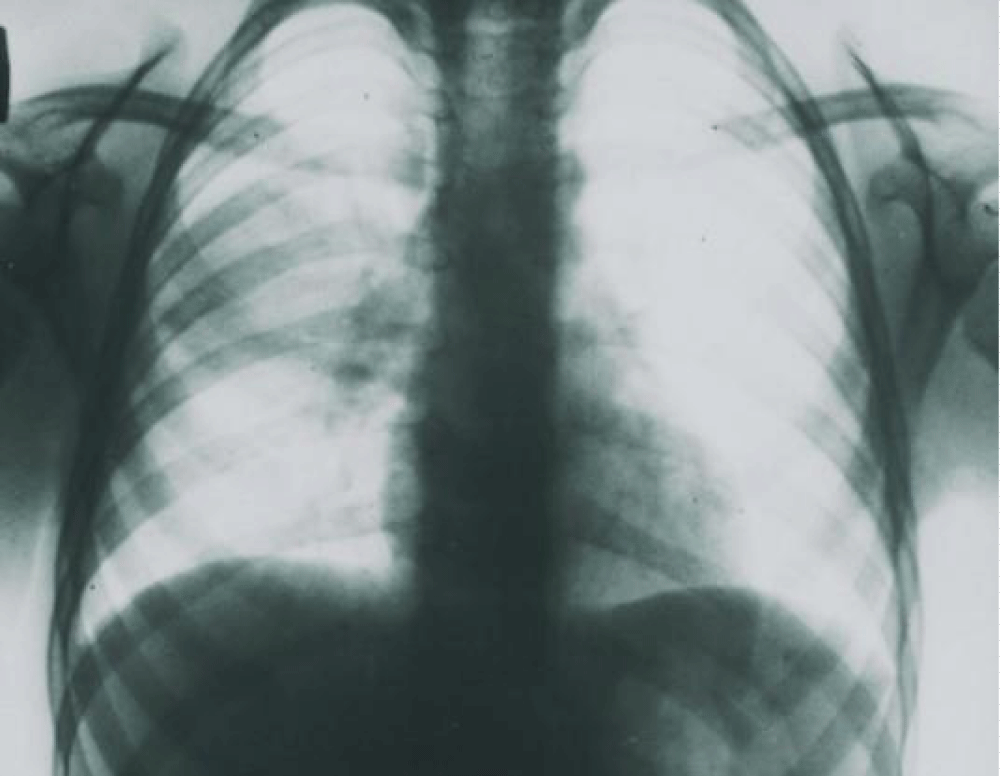
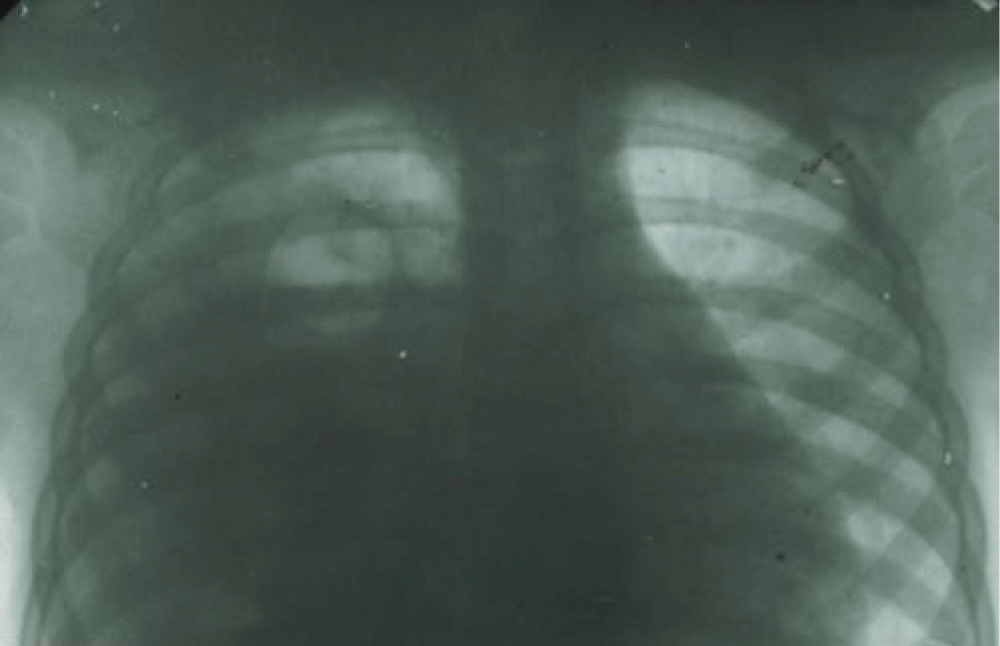
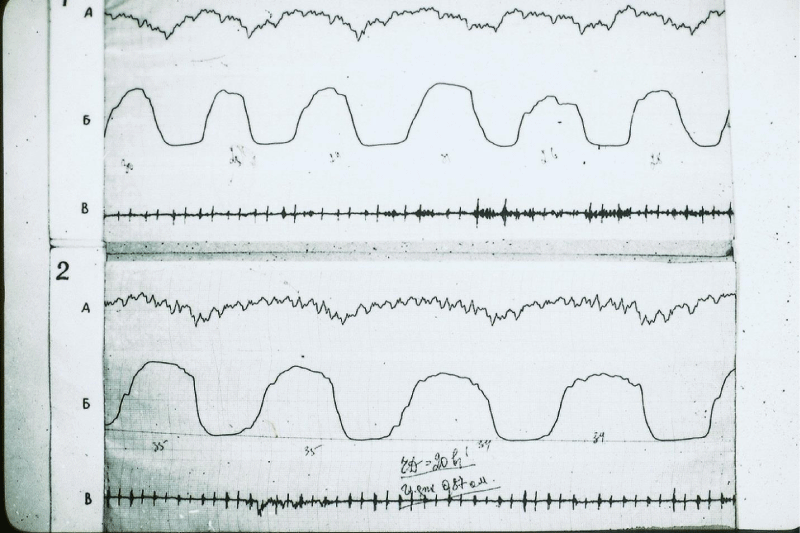
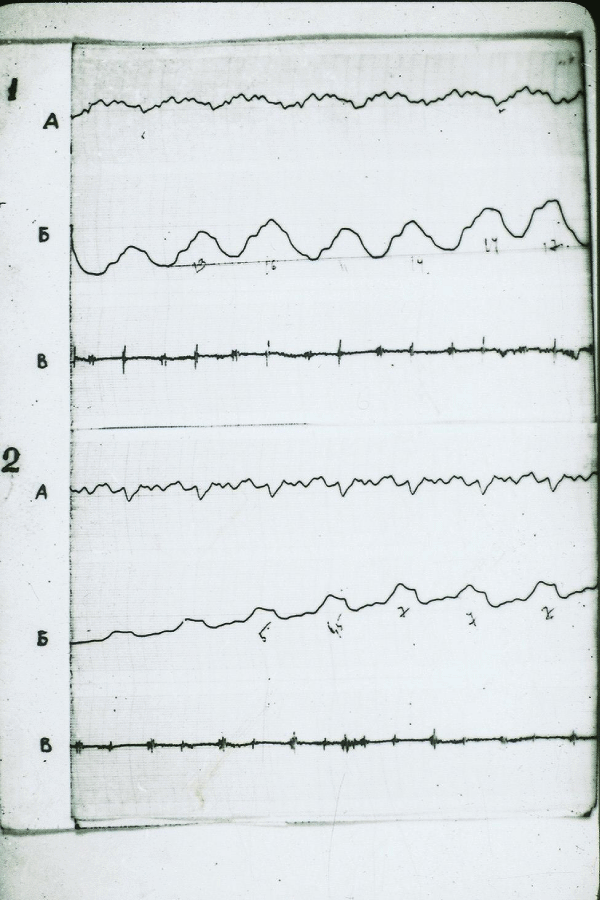
A 2-year-old girl was taken to the clinic with abdominal pain and shortness of breath 12 hours after their appearance. According to the medical history, the child was healthy, but in the last few days, she had a mild respiratory syndrome with a runny nose and cough without fever. Upon admission to the clinic, the patient was diagnosed with AP with signs of so-called intoxication and a tendency to arterial hypotension (Figure 1). Intensive treatment was immediately initiated, including intravenous administration of two antibiotics and intravenous administration of saline solution up to 30 ml/kg/hour for 2 hours, followed by a decrease in the infusion rate to 10 ml/kg/hour. Despite the treatment, the child’s condition did not improve, and a control chest X-ray taken 36 hours after hospitalization was diagnosed with pyopneumothorax (Figure 2). The pus obtained from the pleural cavity during drainage was subjected to bacteriological and microscopic examination, but no microflora was found in it.
Figure 1: X-ray of a 2-year-old girl 12 hours after the detection of the first signs of AP with abdominal pain syndrome. A uniform darkening is observed in the middle right pulmonary field.
Figure 2: X-ray of the same patient (Figure 3), 36 hours after the start of inpatient treatment. There is an intense uniform darkening of almost the entire right hemithorax with a displacement of the mediastinum to the left, as well as a cavity with a fluid level in the upper pulmonary field.
Currently, according to the generally accepted and widespread principles of assessing the condition of patients with AP, the clinical situation described above would be regarded as a septic complication of the inflammatory process in the lung [1-3]. In accordance with the recommendations for diagnosis and treatment, therapeutic efforts will be directed towards empirical isotropic therapy and intensive correction of circulatory disorders using intravenous infusions and vasopressors. In such cases, no importance is attached to such a fundamentally important fact that primary blood flow disorders in patients with AP occur, unlike other inflammatory diseases, in the vessels of the small circulatory circle, and systemic circulatory disorders, which are used as one of the main evaluation criteria, are secondary in patients with this localization of inflammation. At the same time, the fact that blood pressure indicators in the two circulatory circles have an inverse relationship is completely overlooked, and their vital proportions are regulated by reflex and humoral factors with the direct participation of pulmonary vessels in this process [4-8].
Reflex vasospasm of the small circle, which occurs as an excessive protective reaction to growing edema and infiltration of lung tissue and described in previous studies [9], has recently received additional confirmation in the analysis of computed tomograms of the lungs in patients with COVID-19 pneumonia [10,11]. However, established objective evidence of the primary role of blood flow disorders in the pulmonary vascular system and subsequent secondary changes in systemic blood flow does not prevent us from continuing to consider these circulatory shifts in the body of patients with AP as manifestations of sepsis and septic shock. Misconceptions in the interpretation of the mechanisms of circulatory disorders in AP are the cause of overdiagnosis of septic complications in them, which constitute the main group among patients with sepsis [12-14] while differing in the lowest rates of positive microbiological tests [15,16]. In recent years, in the context of the unprecedented growth of viral forms of the disease, the inviolability of the previous concept of AP has led to the automatic transfer of the principles of diagnosis of septic complications to the interpretation of the severity of the condition of such patients without any arguments and confirmations of viral causes [17-21].
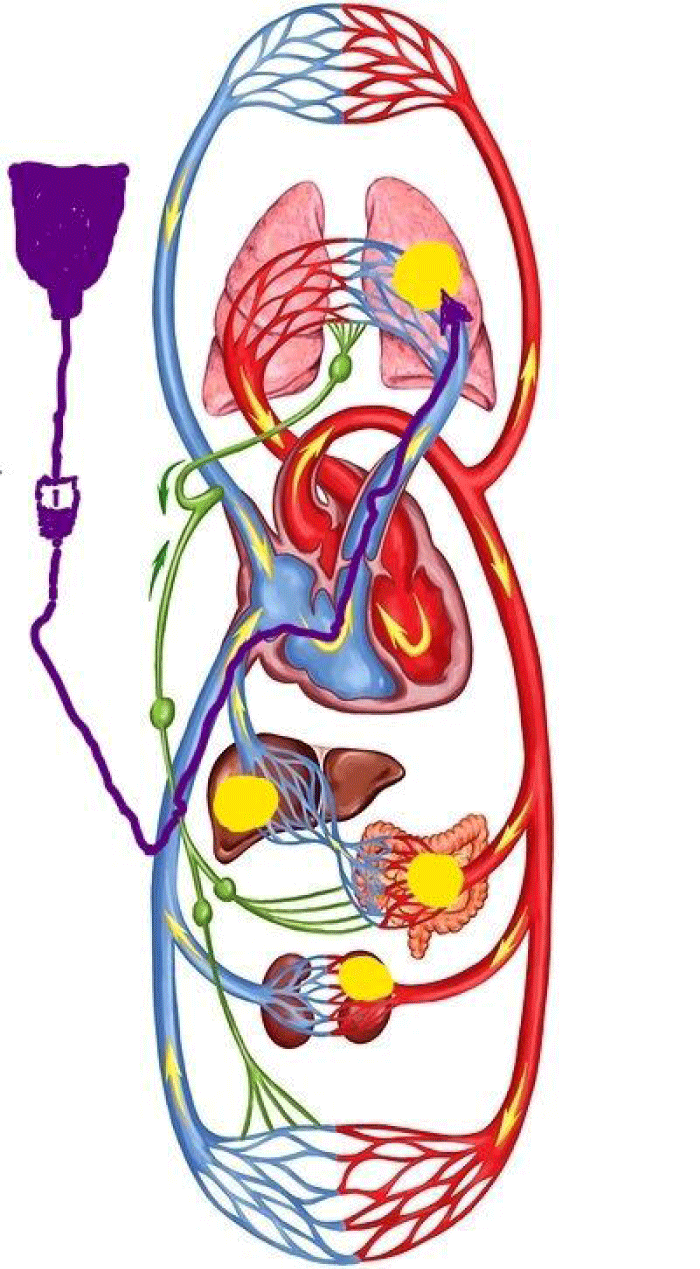
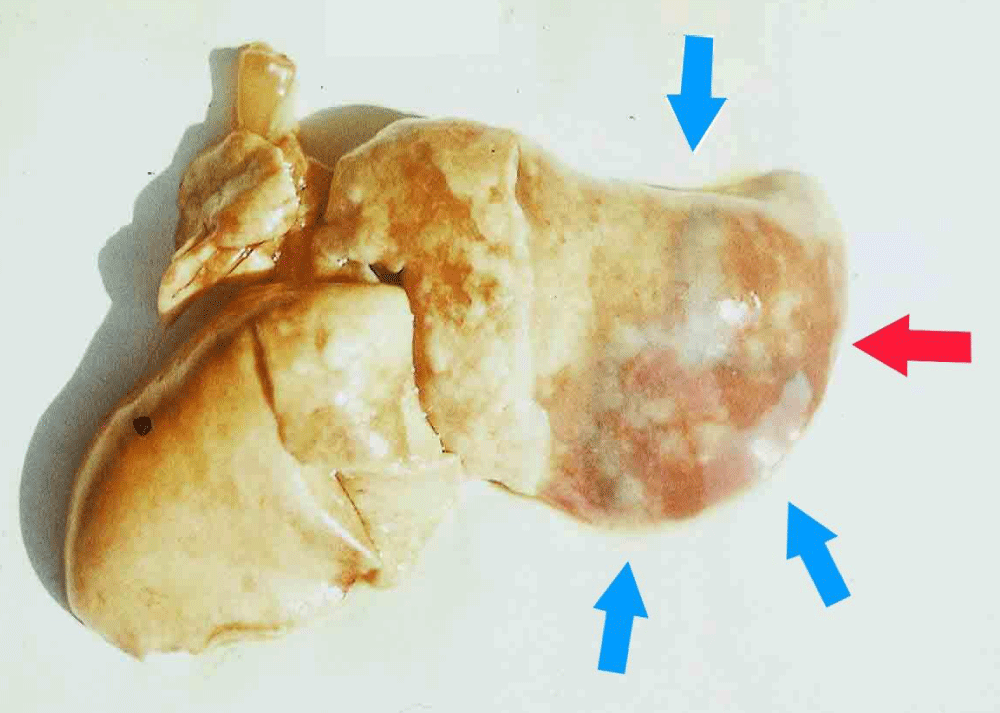
Modern principles of eliminating circulatory disorders that occur already at the earliest stages of AP involve replenishing the volume of circulating blood by intravenous infusion of solutions [18,21]. Regardless of the location of access to the venous bed, this procedure will increase venous return, increasing the overload of the zone of the small circle of blood circulation (Figure 3). Additional confirmation of the negative role of infusions in the initial period of AP was obtained when reproducing the disease in experimental studies [9]. The visual result of the effects of infusions in the experiment is shown in Figure 4.
Figure 3: Schematic representation of the human circulatory system. The initial route of intravenous administration of solutions is shown (dark purple arrow) relative to the foci of acute inflammation (yellow fields), depending on the localization.
Figure 4: Lung macropreparation, experiment. A massive focus of inflammation in the lung (red arrow), surrounded by additional areas of infiltration with a blue tint (blue arrows).
The principles of treatment of aggressive forms of AP that dominate today do not eliminate, but, on the contrary, are capable of stimulating the leading links in the pathogenesis of the disease. This allows us to understand the reasons for the ineffectiveness of such efforts and the increase in the number of observations with complications such as acute respiratory distress syndrome and multiple organ failure. The development of these conditions is based on the preservation of the primary link of vascular disorders in the small circle with a further deepening of shifts in microcirculation in the lung tissue and peripheral organs [9]. Currently, these syndromes do not have real and substantiated prevention plans in practical medicine, since they continue to be considered as consequences of inflammatory agents, and they are trying to present their treatment as a separate autonomous complex [22].
The main misconception of such an autonomous interpretation of such syndromes is that different initial mechanisms of pathogenesis are ultimately capable of leading to identical pathological transformations, which together represent an equivalent set of signs. However, the fundamental difference between the nuances of the formation of the same syndrome in patients with different initial pathologies is that in order to prevent such complications, different therapeutic efforts are required at the early stages of the main nosology. Therefore, the methods of early treatment of patients with AP have their own specifics.
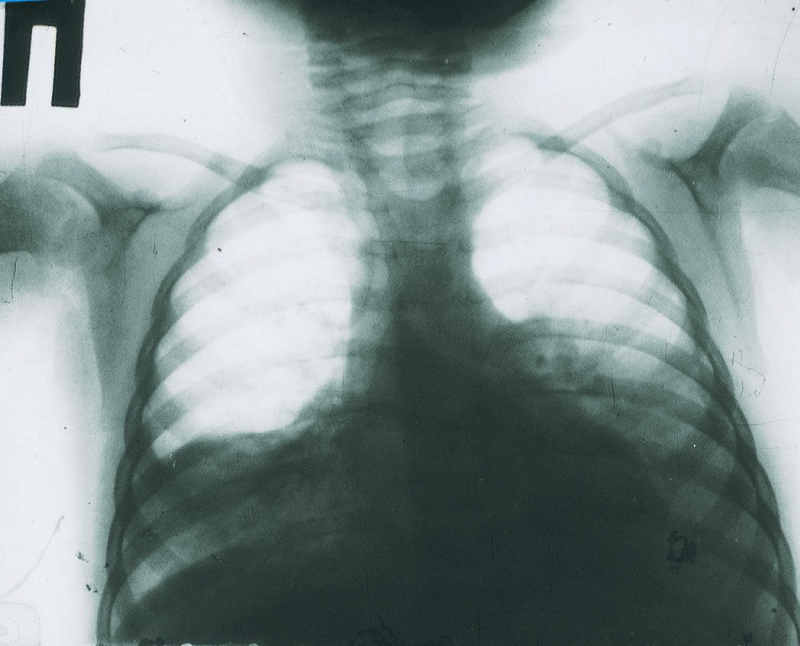
In order for the above-mentioned maxims not to be perceived as unfounded and problematic, the following information should be provided as objective arguments. The revision of ideas about the causes and mechanisms of the development of severe conditions in patients with AP has led to the targeted use of such techniques as cervical vagosympathetic blockade, cupping therapy, or short-term cooling of the patient’s body as first aid. The clinical effect of these procedures looked unambiguous, and the results of the first two techniques were monitored by recording comparative rheopulmonograms [Figures 5,6]. The details of these manipulations and the coincidence of their results were described and published earlier [9], and in this context, they are given only as confirmation of the rule.
Figure 5: Rheogram of ventilation of the patient 8 years old, AP 7-10 segments of the right lung. 1-the original reopulmonography (RPG). 2-RPG after vagosympathetic blockade A-differential RPGs; Б-Main RPG; В-phonocardiogram
Figure 6: Rheogram of pulsatory blood flow of the same patient. The designations are the same.
That protective spasm of the pulmonary vessels, which the body could not independently limit within the limits of permissible changes and turned into a generalized problem, can be eliminated using one of the above procedures with parallel suppression of the vascular inflammatory reaction. As the control records presented above show, immediately after performing the therapeutic manipulation, there is a change in the frequency and intensity of pulse and respiration with the alignment of the disturbed proportions between lung ventilation and blood flow. However, the achieved effect is not enough to completely eliminate the process. An important component of subsequent pathogenetic care for such patients is the constant cleansing of the respiratory tract with the help of such a natural protective mechanism as cough. An active cough restores bronchial peristalsis, which can provide the best drainage of small bronchial branches, the release of which is especially difficult. An increase in intrabronchial pressure during coughing prevents the processes of tissue edema and promotes the reaeration of inflamed areas of the organ [23,24].
An example of the complete opposite of the above observation of approaches to providing medical care to patients with the aggressive development of AP can be one of our following archival descriptions.
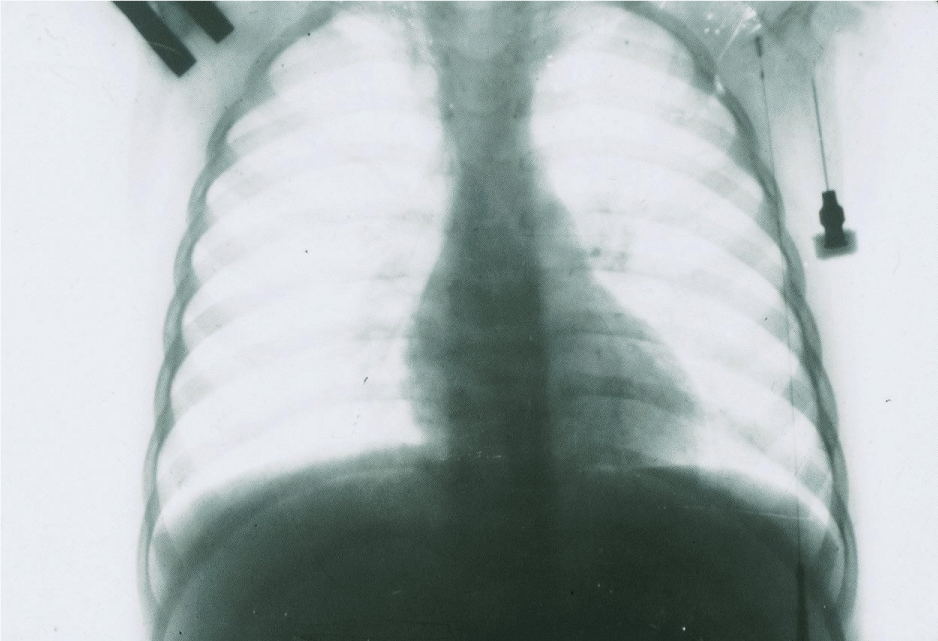
A healthy 22-month-old girl has been showing signs of mild respiratory illness for the past few days without changes in well-being and temperature reaction. Against this background, the day before going to the clinic, there was a sharp deterioration in the condition with hyperthermia, increased cough, and shortness of breath. Shortly before hospitalization, she began complaining of abdominal pain. Preliminary treatment was not carried out.
At the time of hospitalization, massive bilateral pneumonia with a slight thickening of the pleura on the left was diagnosed (Figure 7). Immediately, the patient underwent a vagosympathetic blockade on the left, which was repeated 2 hours later on the right side. For subsequent washing of the tracheobronchial tree and stimulation of cough, a microtracheostomy was performed and steam inhalations were additionally prescribed. Cough stimulation was performed with a frequency of once every 2 hours. No bacteriological study was conducted. Antibacterial therapy included intramuscular injections of penicillin and streptomycin in standard age-related dosages.
Figure 7: X-ray of a 22-month-old patient, 24 hours after the first signs of AP appear. Intense uniform shading in the basal sections of both lungs with moderate thickening of the pleura on the left.
After the start of treatment, the patient’s condition improved significantly, the pain syndrome disappeared, and the body temperature normalized. After 5 days of treatment, there was a complete resolution of the process in both lungs (Figure 8).
Figure 8: X-ray of the same patient (see Figure 7) five days after clinical treatment. Complete restoration of airiness in both lungs.
After the results of the control X-ray, no further antibiotic treatment was carried out. The girl was discharged home with a recommendation to continue the procedures for draining the bronchial tree.
The presented example is a fairly typical observation of a large representative group of patients with aggressive AP development, whose materials were preserved four decades after their treatment. Despite the fact that the leading role of antibiotics at that time did not cause the doubts and contradictions that are currently observed, the antimicrobial section of treatment in this case (see above) was hardly crucial for the rapid achievement of the final result. The routine selection of drugs, which by that time no longer had the same effectiveness, and their use in standard dosages do not give grounds to consider the success of treatment as a result of antibacterial therapy. At the same time, the fundamental rejection of infusion therapy and the use of targeted pathogenetic care are distinctive features of such observations in the group of patients who successfully underwent test treatment.
Currently, despite the numerous inconsistencies and contradictions that are quite obvious between the dominant etiotropic concept of AP and the fundamental foundations of medical science, persistent research continues at the molecular and cellular levels, the main purpose of which remains the search for the necessary counteraction to the causative agent of the process. The desire to find a universal “pneumonia pill” has maintained its intensity over the past decades, despite the likelihood of a large number of non-specific applicants participating in the pneumonia process, the lack of accurate information about the etiology of the disease in most patients and the obvious dependence of the specifics of the disease on functional disorders of the affected organ, without significant dependence on the etiology, even in cases where it can be installed. Focusing on the microstructures of the process and trying to use them to influence the restoration of holistic lung function disorders in an acute process only leads to the loss of precious time and supports misconceptions.
The pathogen of AP, around the virulent properties of which explanations of the specificity and severity of the disease continue to be built today, creates and maintains the illusion that modern science is able to find an effective counteraction to the “main trigger” of nonspecific inflammation at the level of molecular and cellular factors. This trend further deepens the misconception about the problem. On the one hand, the assessment of the condition of patients with AP in general practice continues to be determined by integral indicators of various body functions. It is deviations in vital signs, not molecular shifts, that determine the criteria for the need and urgency of using corrective care products. However, on the other hand, efforts are being made to change the cumulative manifestations of the inflammatory process through indirect exposure through microstructures, which leads to the need to wait for a result and a waste of time. At the same time, the extreme nature of the observed disorders serves as a basis for the use of general therapeutic procedures without taking into account the direction of their impact on pathogenetic mechanisms.
The presented point of view on the current state of the AP problem allows us to understand the reasons for the discrepancy between the growing depth of scientific ideas about the micromechanisms of the disease, on the one hand, and the steady decrease in the effectiveness of treatment of this group of patients, on the other. Changes in the basic conditions and features of acute inflammatory processes of non-specific etiology in the lung tissue, which have become one of the characteristic features of the entire period of antibiotic use, have now reached a situation where professional ideas about the essence of these diseases require a comprehensive analysis and cardinal correction. The preservation of established traditions in this area of medicine is fraught with further deterioration of the situation, especially since the cause of all the observed etiological transformations in the face of antibiotics ceases to play the seemingly irreplaceable role that they played in previous years.
- Murillo-Zamora E, Medina-González A, Zamora-Pérez L, Vázquez-Yáñez A, Guzmán-Esquivel J, Trujillo-Hernández B. Performance of the PSI and CURB-65 scoring systems in predicting 30-day mortality in healthcare-associated pneumonia. Med Clin (Barc). 2018 Feb 9;150(3):99-103. English, Spanish. doi: 10.1016/j.medcli.2017.06.044. Epub 2017 Aug 1. PMID: 28778682.
- Ilg A, Moskowitz A, Konanki V, Patel PV, Chase M, Grossestreuer AV, Donnino MW. Performance of the CURB-65 Score in Predicting Critical Care Interventions in Patients Admitted with Community-Acquired Pneumonia. Ann Emerg Med. 2019 Jul;74(1):60-68. doi: 10.1016/j.annemergmed.2018.06.017. Epub 2018 Aug 2. PMID: 30078659; PMCID: PMC6359992.
- Chen J, Liu B, Houwei D. Performance of CURB-65, PSI, and APACHE-II for predicting COVID-19 pneumonia severity and mortality. European Journal of Inflammation.2021; 19. https://doi.org/10.1177/20587392211027083
- Schwiegk H. Der Lungenentlastungsreflex. Pflügers Arch. ges. Physiol. 1935; 236: 206-219.
- Osorio J, Russek M. Reflex Changes on the Pulmonary and Systemic Pressures Elicited by Stimulation of Baroreceptors in the Pulmonary Artery. Circulation Research, 1968; X: 664-667.
- Olivia V. Cardiology secrets. Chapter 41, p. 210. Adair Edition: 2, illustrated Published by Elsevier Health Sciences. 2001; ISBN 1-56053-420- 6: 978-1-56053-420.
- Colledge NR, Walker BR, Ralston SH, Britton R. eds. Davidson's Principles and Practice of Medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. 2010; ISBN 978-0-7020-3084-0.
- Normal Hemodynamic Parameters – Adult. Edwards Lifesciences LLC. Archived from the original on 2010-11-10.
- Klepikov I. The Didactics of Acute Lung Inflammation. Cambridge Scholars Publishing. 2022; 320. ISBN: 1-5275-8810-6, ISBN13: 978-1- 5275-8810-3.
- Thillai M, Patvardhan C, Swietlik EM, McLellan T, De Backer J, Lanclus M, De Backer W, Ruggiero A. Functional respiratory imaging identifies redistribution of pulmonary blood flow in patients with COVID-19. Thorax. 2021 Feb;76(2):182-184. doi: 10.1136/thoraxjnl-2020-215395. Epub 2020 Aug 28. PMID: 32859733.
- Dierckx W, De Backer W, Lins M, De Meyer Y, Ides K, Vandevenne J, De Backer J, Franck E, Lavon BR, Lanclus M, Thillai M. CT-derived measurements of pulmonary blood volume in small vessels and the need for supplemental oxygen in COVID-19 patients. J Appl Physiol (1985). 2022 Dec 1;133(6):1295-1299. doi: 10.1152/japplphysiol.00458.2022. Epub 2022 Oct 21. PMID: 36269576; PMCID: PMC9722246.
- Mayr FB, Yende S, Angus DC. Epidemiology of severe sepsis. Virulence. 2014 Jan 1;5(1):4-11. doi: 10.4161/viru.27372. Epub 2013 Dec 11. PMID: 24335434; PMCID: PMC3916382.
- Kaukonen KM, Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med. 2015 Apr 23;372(17):1629-38. doi: 10.1056/NEJMoa1415236. Epub 2015 Mar 17. PMID: 25776936.
- Cillóniz C, Torres A, Niederman MS. Management of pneumonia in critically ill patients. BMJ. 2021 Dec 6;375:e065871. doi: 10.1136/bmj-2021-065871. PMID: 34872910.
- Waterer GW, Quasney MW, Cantor RM, Wunderink RG. Septic shock and respiratory failure in community-acquired pneumonia have different TNF polymorphism associations. Am J Respir Crit Care Med. 2001 Jun;163(7):1599-604. doi: 10.1164/ajrccm.163.7.2011088. PMID: 11401880.
- Sanjay S. Community-Acquired Pneumonia. MSD Manual, Professional Version. Last full review/revision. 2020. https://www.msdmanuals.com/en-in/professional/pulmonary-disorders/pneumonia/community-acquired-pneumonia
- Lin GL, McGinley JP, Drysdale SB, Pollard AJ. Epidemiology and Immune Pathogenesis of Viral Sepsis. Front Immunol. 2018 Sep 27;9:2147. doi: 10.3389/fimmu.2018.02147. PMID: 30319615; PMCID: PMC6170629.
- Schlapbach LJ, Kissoon N, Alhawsawi A, Aljuaid MH, Daniels R, Gorordo-Delsol LA, Machado F, Malik I, Nsutebu EF, Finfer S, Reinhart K. World Sepsis Day: a global agenda to target a leading cause of morbidity and mortality. Am J Physiol Lung Cell Mol Physiol. 2020 Sep 1;319(3):L518-L522. doi: 10.1152/ajplung.00369.2020. Epub 2020 Aug 19. PMID: 32812788.
- Rollas K, Ersan G, Zincircioğlu. Septic shock in patients admitted to intensive care unit with COVID-19 pneumonia. Eurasian J Pulmonol. 2021; 23:95-100.
- Roger C. COVID-19: should we consider it as a septic shock? (The treatment of COVID-19 patients in the ICU). Curr Opin Anaesthesiol. 2021 Apr 1;34(2):119-124. doi: 10.1097/ACO.0000000000000956. PMID: 33470663.
- Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, Mcintyre L, Ostermann M, Prescott HC, Schorr C, Simpson S, Wiersinga WJ, Alshamsi F, Angus DC, Arabi Y, Azevedo L, Beale R, Beilman G, Belley-Cote E, Burry L, Cecconi M, Centofanti J, Coz Yataco A, De Waele J, Dellinger RP, Doi K, Du B, Estenssoro E, Ferrer R, Gomersall C, Hodgson C, Møller MH, Iwashyna T, Jacob S, Kleinpell R, Klompas M, Koh Y, Kumar A, Kwizera A, Lobo S, Masur H, McGloughlin S, Mehta S, Mehta Y, Mer M, Nunnally M, Oczkowski S, Osborn T, Papathanassoglou E, Perner A, Puskarich M, Roberts J, Schweickert W, Seckel M, Sevransky J, Sprung CL, Welte T, Zimmerman J, Levy M. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021 Nov;47(11):1181-1247. doi: 10.1007/s00134-021-06506-y. Epub 2021 Oct 2. PMID: 34599691; PMCID: PMC8486643.
- Hammond NE, Finfer S. Can we design better ARDS trials? Thorax. 2023 Oct;78(10):955-956. doi: 10.1136/thorax-2023-220446. Epub 2023 Jul 26. PMID: 37495366.
- Cough. Wikipedia. https://en.wikipedia.org/wiki/Cough
- McCool FD. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006 Jan;129(1 Suppl):48S-53S. doi: 10.1378/chest.129.1_suppl.48S. PMID: 16428691.