More Information
Submitted: August 01, 2023 | Approved: August 16, 2023 | Published: August 17, 2023
How to cite this article: Lima E. Cardiac Tamponade as the Cause of Pulmonary Edema: Case Report. J Pulmonol Respir Res. 2023; 7: 021-023.
DOI: 10.29328/journal.jprr.1001046
Copyright License: © 2023 Lima E. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Cardiac tamponade; Bedside echocardiogram; Point of care ultrasound; Pericardiocentesis; Lung ultrasound
Cardiac Tamponade as the Cause of Pulmonary Edema: Case Report
Emídio Lima*
Emergency Department, Roberto Santos General Hospital, Salvador, Brazil
*Address for Correspondence: Emídio Lima, Professor, Ph.D, MD, Emergency Department, Roberto Santos General Hospital, Salvador, Brazil, Email: [email protected]
Introduction: Cardiac tamponade is an emergency syndrome that requires fast diagnosis and treatment; otherwise patient follows obstructive shock and cardiac arrest.
Case report: A 70-year-old female was brought to the emergency department with hypoxemia. She had a history of progressive dyspnea over the past three weeks. Past medical history includes smoking. On physical examination: tachypnea, hypoxemia (SaO2 89%), jugular venous distention, arterial pressure 220/100 mmHg, heart rate rhythmic of 82 bpm. On pulmonary auscultation: diffuse and bilateral crackles. Lung ultrasound showed a bilateral B line and the echocardiogram demonstrated a pericardial effusion with signs of tamponade. A pericardiocentesis evacuated 620 ml of hemorrhagic fluid and the patient was transferred to the intensive care unit, hemodynamically stable, with SaO2 95%. At the ICU the echocardiogram, showed resolution of the cardiac tamponade and a tumor adhered to the lateral wall of the left ventricle. Chest CT demonstrated: a left lung tumor, infiltrating the pericardial sac. A pericardium biopsy demonstrated undifferentiated carcinoma.
Discussion: Cardiac tamponade diagnosis requires a high level of suspicion. Respiratory failure, chest pain, and shock, observed in cardiac tamponade, are also present in different diseases. The most common finding of cardiac tamponade is dyspnea (78% of cases). Our patient had dyspnea due to pulmonary edema, secondary to left ventricle diastolic dysfunction caused by the tamponade. A bedside echocardiogram made the diagnosis of cardiac tamponade and guided the effective pericardiocentesis.
Conclusion: Cardiac tamponade must be suspected in all cases of acute dyspnea. Echocardiogram is the method of choice for the diagnosis and for guiding the pericardiocentesis.
Cardiac tamponade is an emergency syndrome that requires fast diagnosis and treatment; otherwise patient follows obstructive shock and cardiac arrest due to pulseless electrical activity or asystole.
The Beck’s triad, hypotension, jugular venous distention, and muffled heart sounds can be absent in 14% of the patients with cardiac tamponade [1]. Manifestations such as pulmonary edema or angina may occur without hypotension [2]. Patients with hypovolemia and cardiac tamponade can have hypotension without jugular venous distention [1] .
Cardiac effusion complicated with tamponade can occur in many conditions such as malignant disease in the advanced phase, myocardial infarction, renal failure with uremia, connective tissue disorder, drug-related lupus, cardiovascular surgery or coronary intervention, thoracic trauma, pacemaker lead implantation, central venous catheter insertion, HIV, and tuberculosis [3].
The unique and effective treatment of the cardiac tamponade is drainage of pericardial effusion (pericardiocentesis or pericardial window) [4,5].
We describe a case of cardiac tamponade whose initial diagnosis was respiratory failure due to pulmonary edema, characterized by shortness of breath, hypoxemia, and bilateral pulmonary crackles, in a 70-year-old female. We have the patient’s consent for the publication of her case.
Clinical findings
A 70-year-old black female was brought to our emergency department with respiratory distress. On admission, she complained of progressive dyspnea, initially during moderate physical activity, over the past three weeks, associated with orthopnea, paroxysmal nocturnal dyspnea, and edema in her legs. The past medical history includes bipolar disorder and smoking. Upon physical examination, she had tachypnea (respiratory rate of 25 breaths per minute), hypoxemia (SaO2 89%), jugular venous distention, arterial pressure 220/100 mmHg, heart rate rhythmic of 82 beats per minute, axillary temperature of 36.1 ºC. Diffuse and bilateral crackles on pulmonary auscultation. There was edema in both legs and on abdominal examination there were no signs of peritoneal irritation. Respiratory support was initiated with oxygen, 2 liters per minute, delivered through the nasal catheter. The oxygen saturation increased to 95%.
Diagnosis
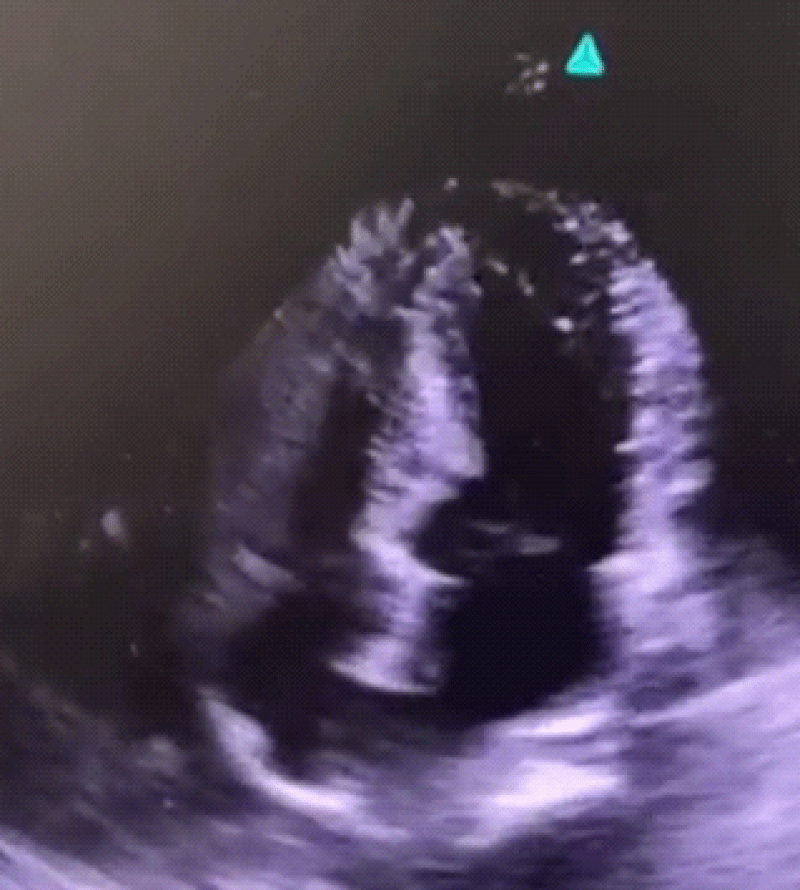
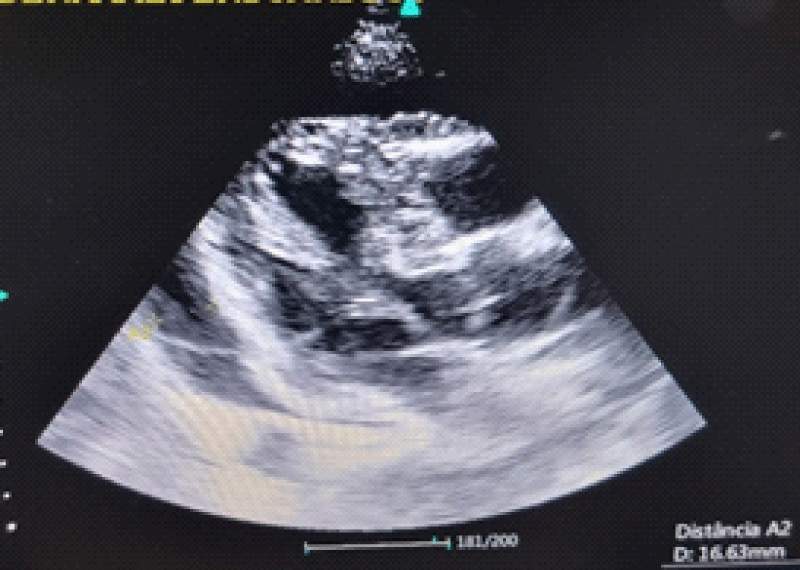
A bedside lung ultrasound showed a bilateral B line pattern compatible with pulmonary edema and the echocardiogram demonstrated a large pericardial effusion with signs of tamponade (Figures 1,2).
Figure 1: Pericardial effusion with tamponade sign – right ventricular diastolic collapse.
Figure 2: Pericardial effusion in parasternal long-axis window.
Treatment
A bedside, subcostal pericardiocentesis, under local anesthesia, was done and approximately 570 ml of hemorr-hagic fluid was evacuated. After that, the patient’s tachypnea decreases. More than 50 ml of hemorrhagic pericardial fluid was evacuated and the patient was transferred to the intensive care unit (ICU), hemodynamically stable, without vasopressor, and with SaO2 95%.
Outcome
At the ICU the echocardiogram was repeated, showing resolution of the cardiac tamponade and a tumor adhered to the lateral wall of the left ventricle. One chest CT was ordered, whose findings were: left lung tumor, measuring 5.5 × 5 cm, on the inferior lobe, infiltrating pericardial sac. A pericardial fluid sample sent for cytology analysis was negative for bacteria, fungus, or virus, but positive for malignancy. A pericardium biopsy analyzed by pathology demonstrated undifferentiated carcinoma. Considering the diagnosis, of advanced malignancy, the patient was moved to palliative care. She progressively deteriorated her oxygenation and died due to tumor infiltration in both lungs.
Cardiac tamponade diagnosis, in non-traumatic patients requires a high level of suspicion. Respiratory failure, chest pain, and shock, observed in cardiac tamponade, are also present in different diseases such as pulmonary edema, pulmonary embolism, myocardial infarction, and pneumonia [2,6]. The most common finding of cardiac tamponade is dyspnea (78% of cases) [2] and the most frequent clinical presentation is dyspnea, tachycardia, and elevated venous jugular pressure [3]. Our patient had dyspnea and, on lung ultrasound, was observed an interstitial-alveolar syndrome; it is characterized by bilateral and diffuse B lines and represents pulmonary edema. Pulmonary edema is one of the manifestations of hemodynamic instability, secondary, in cardiac tamponade, to left ventricular diastolic dysfunction due to left ventricular diastolic collapse. After the diagnosis of pulmonary edema, by pulmonary echography, a bedside echocardiogram demonstrated that cardiac tamponade was the pathophysiology related to our case. Echocardiography is a non-invasive tool, with high accuracy for cardiac tamponade diagnosis, and a bedside approach, preventing the risks of patient’s transference to the imaging department. We can use an echocardiogram for excluding diagnoses such as cardiomyopathy, constrictive pericarditis, and myocardial infarction in critically ill patients [7]. The diagnosis of cardiac tamponade, by echocardiography, is done when observed: a pericardial effusion with right atrial and right ventricular diastolic collapse [3,6]. The four most frequent etiologies of cardiac tamponade are cancer (30% - 60%), uremia (10% - 15%), idiopathic pericarditis (5% - 15%), and infectious disease (5% - 10%) [3] Table 1 [8]. In our patient, the cytology review of the pericardial fluid, the sensitivity of 75% [9-11] and the pericardium biopsy confirmed malignancy as the etiology of the pericardium effusion and tamponade. In general, malignancy causes pericardium effusion due to direct invasion of the advanced mediastinum or lung tumor [2]. An advanced lung cancer invading the pericardium sac was diagnosed in our case.
| Table 1: Etiologies of pericardial tamponade. | |
| Etiology | Incidence rates (%) |
| Malignant diseases | 30 - 60 |
| Uremia | 10 - 15 |
| Idiopathic pericarditis | 5 - 15 |
| Infectious diseases | 5 - 10 |
| Anticoagulation | 5 - 10 |
| Connective tissue diseases | 2 - 6 |
| Dressler or postpericardiotomy syndrome | 1 - 2 |
Cardiac tamponade must be suspected in all cases of acute dyspnea. If that diagnosis is confirmed emergency pericardial effusion drainage, pericardiocentesis, or pericardial window, must be done.
Echocardiogram, at the bedside, is the method of choice for the diagnosis of cardiac tamponade, and it is also a necessary approach for guiding safe pericardial effusion drainage.
- Demetriades D. Cardiac wounds. Experience with 70 patients. Ann Surg. 1986 Mar;203(3):315-7. doi: 10.1097/00000658-198603000-00018. PMID: 3954485; PMCID: PMC1251098.
- Scheinin SA, Sosa-Herrera J. Case report: cardiac tamponade resembling an acute myocardial infarction as the initial manifestation of metastatic pericardial adenocarcinoma. Methodist Debakey Cardiovasc J. 2014 Apr-Jun;10(2):124-8. doi: 10.14797/mdcj-10-2-124. PMID: 25114766; PMCID: PMC4117332.
- Yarlagadda C. Cardiac tamponade: practice, essentials, background and pathophysiology. http://emedicine.medscape.com/article/152083- overview#showall
- Stashko E, Meer JM. Cardiac Tamponade. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK431090/.
- Martins QC, Juliano C. Pericardial Effusion and Cardiac Tamponade: Etiology and Evolution in the Contemporary Era. Int J Cardiovasc Sci. 25/out/2021. 34(5 supl 1) 24-31.
- Bottinor W, Fronk D, Sadruddin S, Foster H, Patel N, Prinz A, Jovin IS. Acute Cardiac Tamponade in a 58-Year-Old Male with Poststreptococcal Glomerulonephritis. Methodist Debakey Cardiovasc J. 2016 Sep;12(3):175-176. doi: 10.14797/mdcj-12-3-175. PMID: 27826373; PMCID: PMC5098576.
- Chong HH, Plotnick GD. Pericardial effusion and tamponade: evaluation, imaging modalities, and management. Compr Ther. 1995 Jul;21(7):378-85. PMID: 7554815.
- Lima E. Cardiac Tamponade as Cause of Respiratory Distress and Cardiac Arrest. J.Clin Case Stu. 2018; 3(3): dx.doi.org/10.16966/24714925.174
- Petcu DP, Petcu C, Popescu CF, Bătăiosu C, Alexandru D. Clinical and cytological correlations in pericardial effusions with cardiac tamponade. Rom J Morphol Embryol. 2009;50(2):251-6. PMID: 19434319.
- Cornily JC, Pennec PY, Castellant P, Bezon E, Le Gal G, Gilard M, Jobic Y, Boschat J, Blanc JJ. Cardiac tamponade in medical patients: a 10-year follow-up survey. Cardiology. 2008;111(3):197-201. doi: 10.1159/000121604. Epub 2008 Apr 25. PMID: 18434725.
- Barra LD. Acute cardiac tamponade: a brief review. Medical Journal of Minas Gerais. 2008; 18(3 supl 4): S37-S40.