More Information
Submitted: July 13, 2021 | Approved: July 29, 2021 | Published: July 30, 2021
How to cite this article: Khanduja D, Pandhi N, Pulmonary mucormycosis in post-pulmonary tuberculosis as an emerging risk factor: A rare case report. J Pulmonol Respir Res. 2021; 5: 059-063.
DOI: 10.29328/journal.jprr.1001026
Copyright License: © 2021 Khanduja D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pulmonary mucormycosis; Tuberculosis; HIV; Air crescent sign
Pulmonary mucormycosis in post-pulmonary tuberculosis as an emerging risk factor: A rare case report
Divya Khanduja1* and Naveen Pandhi2
1Junior Resident, Department of Pulmonary Medicine, Government Medical College, Amritsar, Punjab, India
2Professor and Head, Department of Pulmonary Medicine, Government Medical College, Amritsar, Punjab, India
*Address for Correspondence: Divya Khanduja, Junior Resident, Department of Pulmonary Medicine, Government Medical College, Amritsar, Punjab, India, Tel: 9582969172; Email: [email protected]
Pulmonary mucormycosis is an uncommon pulmonary fungal disease, which is commonly seen in immunocompromised individuals. It is caused by fungi of class Zygomycetes. It constitutes the third most common invasive fungal infection following aspergillosis and candidiasis. Risk factors include patients with hematological malignancies, diabetes mellitus, and immunocompromised states. It is difficult to diagnose early due to non-specific clinical presentation and delay in treatment associated with greater mortality. As we know that Tuberculosis and HIV are highly prevalent in country like India. Post pulmonary tuberculosis is emerging as a risk factor for Pulmonary mucormycosis in the developing countries like India. Patients with non-resolving pneumonia are generally misdiagnosed as Pulmonary tuberculosis. The diagnosis of Pulmonary Mucormycosis is based upon demonstration of fungal hyphae in the clinical specimen. We highlight the importance of clinical suspicion in these cases for early diagnosis and early treatment initiation can reverse morbidity and mortality associated with Pulmonary Mucormycosis. We report 2 cases of Pulmonary mucormycosis present in post-pulmonary tuberculosis patients.
Pulmonary mucormycosis is a rare disease caused by order Mucorales of class Zygomycetes, affecting immunocompromised individuals, both in developing and developed countries [1]. The term Zygomycosis, which was used for infections caused by fungi of the order Mucorales, has been discarded according to the recent taxonomic literature that abolished Zygomycetes as a class [2]. Mucorales fungi are ubiquitous, saprophytic and not fastidious fungi found on soil or decaying organic matter. The three genera that are most commonly associated with infections in the human, namely, Rhizopus, Mucor and Absidia (Lichtheimia) [3]. Rhino-orbital-cerebral and pulmonary infections are the most common manifestations caused by these fungi by the inhalation of spores. In 1876, the first case of Pulmonary mucormycosis was reported by Furbringer [4]. The prevalence of mucormycosis is estimated to be around 70 times higher in India than globally. Diabetes mellitus is the most common risk factor, followed by haematological malignancy and solid-organ transplant. Other risk factors include illicit use of intravenous drugs, prolonged steroid use, persistent neutropenia, desferoxamine therapy. Patients with post-pulmonary tuberculosis and chronic kidney disease are additional emerging risk factors for developing mucormycosis in India [5]. There is spike in the cases of Mucormycosis due to COVID-19 infection as it is associated with impaired immune status in the infected patient.
A 26-year-old male presented at emergency with complaints of cough with mucopurulent sputum and breathlessness for 2 months, haemoptysis and fever for 7 days. He was diagnosed with HIV 1-year back for which patient is on ART (anti-retroviral therapy) as patient has past history of intravenous drug abuse (heroin addict) 1year back for the duration of 9 months. He was treated for pulmonary tuberculosis thrice in past 3 years. He gave history of smoking for 4-5 years, alcoholic for 5 years. He was taking anti-tubercular treatment (Rifampicin, Isoniazid, Ethambutol, Pyrazinamide) for Pulmonary tuberculosis on clinico-radiological basis for last 10 days.
On examination, patient was emaciated. He was slight dyspnoeic without the use of accessory muscles, with a blood pressure of 120/70 mmHg, pulse rate of 94/min, respiratory rate of 26/min, and saturation of 92% on room air. On general physical examination, clubbing was present. On auscultation, bilateral bronchial breath sounds present on interscapular and infra-scapular areas increase vocal fremitus bilaterally.
Laboratory findings revealed haemoglobin of 12 g/dl, white blood count of 6,400, ESR-71, RBS-110 mg/dl, serum bilirubin-0.5, SGOT-45, SGPT-38, TSP-6.4, DSP-3.7, serum creatinine-0.8. His sputum for AFB on Ziehl-Neelson staining and gram stain and culture were negative. Induced sputum for fungus revealed fungal hyphae on KOH mount. Sputum for CBNAAT (Xpert MTB/RIF) showed MTB not detected. The nasopharyngeal swab sent for COVID-19 RTPCR testing was negative. Serology of HBsAg and HCV were negative.
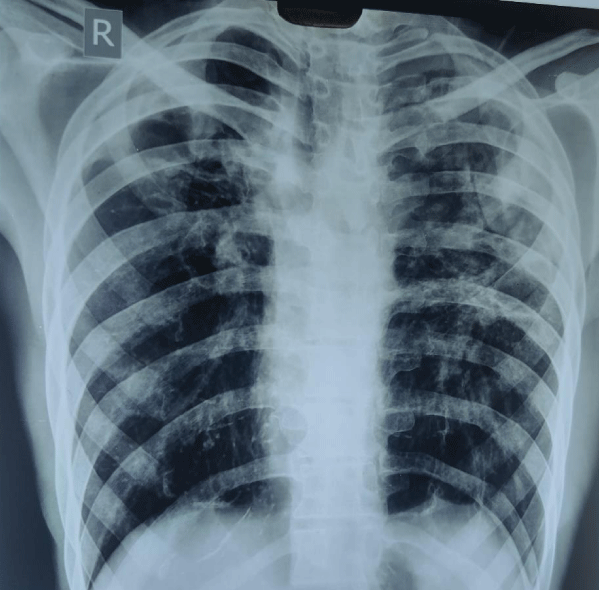
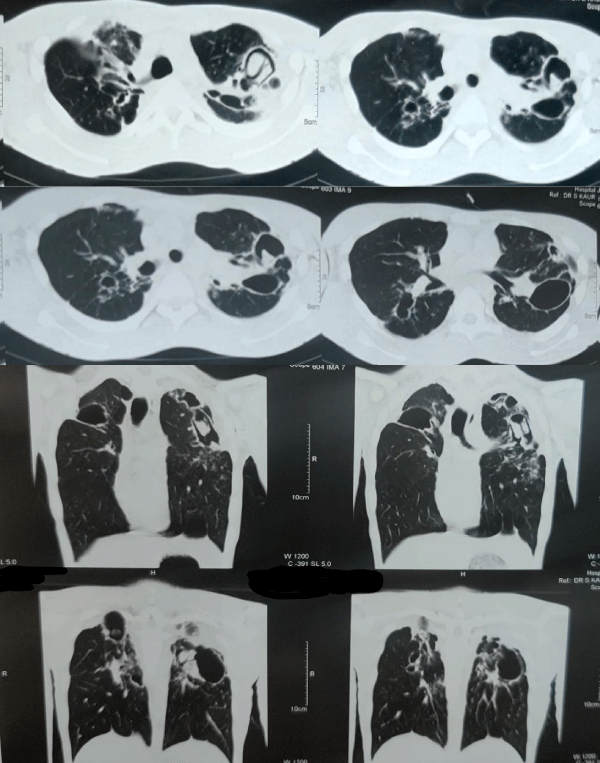
Chest radiograph (Figure 1) showed bilateral heterogenous opacities on upper and middle zones bilaterally. Computed tomography (Figure 2) revealed multifocal areas of cavitation involving bilateral upper and lower lobes of lungs. Fungal balls in bilateral upper lobe cavities showing air crescent sign.
Figure 1: CXR PA view showed bilateral heterogenous opacities on upper and middle zones of both sides.
Figure 2: CECT Chest showed multifocal areas of cavitation involving bilateral upper and lower lobes of lungs. Fungal balls in bilateral upper lobe cavities showing air crescent sign.
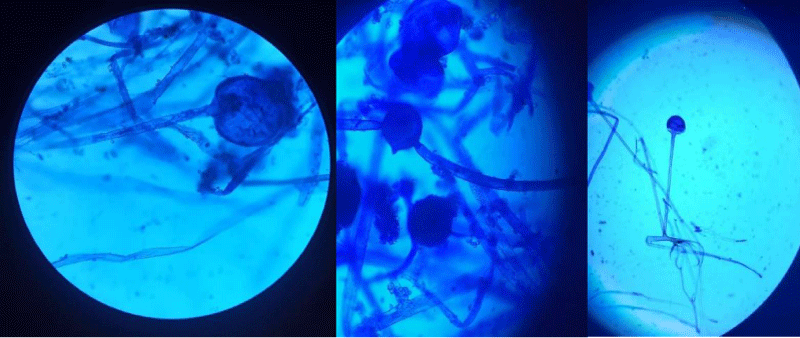
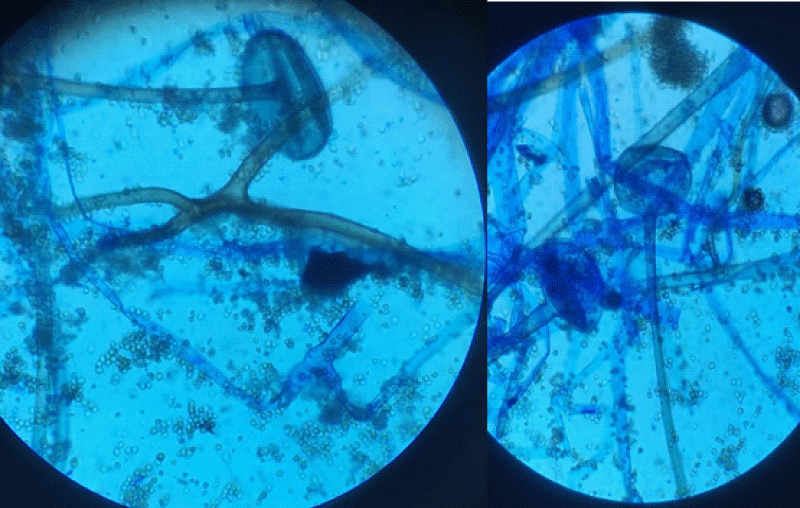
Owing to the unaffordability of patient, the patient denied for Bronchoscopy which was advised to him. Transthoracic needle aspiration from left-sided cavitary lesion was done, and aspirated sample sent for AFB smear, gram stain and culture, malignant cells and fungal smear examination. Aspirate was found to be negative for AFB and malignant cells. On KOH mount, (Figure 3) we found broad aseptate thin-walled fungal hyphae with right angle branching, Rhizopus genus was found. Patient was started on intravenous Amphotericin-B at the dose of 5 mg/kg/day, patient was referred to cardiothoracic surgery department for further planned left sided upper lobectomy of patient.
Figure 3: KOH mount showed broad aseptate thin-walled fungal hyphae with right angle branching, found to be genus Rhizopus.
A 55-year-old female presented at emergency with complaints of cough with mucopurulent sputum and breathlessness for past 4 weeks, and haemoptysis for past 7 days. There was no history of fever, chest pain or bleeding from any other sites. There was no history of weight loss or night sweats. She gave history of Pulmonary tuberculosis for which took anti-tubercular treatment twice 5 years back. She was non-diabetic and non-hypertensive. There was no history of any drug intake.
On examination, patient was slightly dyspnoeic without any use of accessory muscles, with a blood pressure of 128/70 mmHg, pulse rate of 98/min, respiratory rate of 30/min, and saturation of 90% on room air. On general physical examination, pallor was present. On auscultation, bilateral bronchial breath sounds present on interscapular and infra-scapular areas with increase in vocal resonance bilaterally.
Laboratory findings revealed haemoglobin of 10 g/dl, white blood count of 7,800, ESR-48, RBS-106 mg/dl, serum bilirubin-0.5, SGOT-31, SGPT-28, TSP-5.4, DSP-2.7, serum creatinine-0.8. Her sputum for AFB on Ziehl-Neelson staining and gram stain and culture were negative. Induced sputum for fungus revealed fungal hyphae on KOH mount. Sputum for CBNAAT (Xpert MTB/RIF) showed MTB not detected. The nasopharyngeal swab sent for COVID-19 RTPCR testing was negative. Serology of HIV was negative.
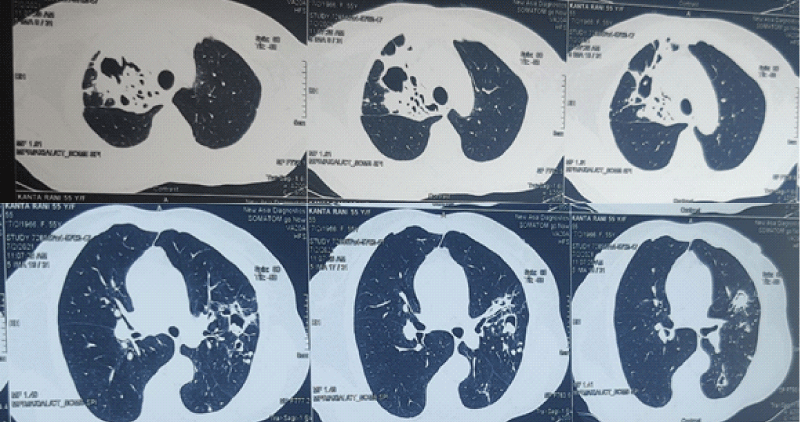
Computed tomography chest (Figure 4) revealed consolidative cavitary lesions showing intra-cavitary fungal balls as air crescent sign at right upper lobe, posterior segment of left upper lobe and superior segment of left lower lobe.
Figure 4: Revealed consolidative cavitary lesions showing intra-cavitary fungal balls as air crescent sign at right upper lobe, posterior segment of left upper lobe and superior segment of left lower lobe.
Transthoracic needle aspiration from right-sided cavitary lesion was done, and aspirated sample sent for AFB smear, gram stain and culture, malignant cells and fungal smear examination. Aspirate was found to be negative for AFB and malignant cells. On KOH mount, (Figure 5) we found broad aseptate thin-walled fungal hyphae with right angle branching, Rhizopus genus was found. Patient was started on intravenous Amphotericin-B at the dose of 5 mg/kg/day, patient was referred to cardiothoracic surgery department for further planned right sided upper lobectomy of patient.
Figure 5: KOH mount showed broad aseptate thin-walled fungal hyphae with right angle branching, found to be genus Rhizopus..
Mucormycosis is an opportunistic, angio-invasive fungal infection, affecting immunocompromised individuals. It is a rapidly progressive infection associated with high morbidity and mortality. In recent years, it has been observed that the epidemiology of mucormycosis is being changing as incidence has raised with new causative agents and changing susceptible population. It is very high in Asian countries as compared globally. Though diabetes mellitus is most common risk factor found in Asia as well as globally, post-tuberculosis and chronic renal failure are new risk groups emerging in developing countries. The rhino-orbital-cerebral form of mucormycosis is most commonly associated with diabetes mellitus, whereas, pulmonary mucormycosis seen in patients with haematological malignancy and transplant recipients [6]. Other risk factors include illicit use of intravenous drugs, prolonged steroid use, persistent neutropenia, desferoxamine therapy. In India, Post-covid mucormycosis cases have also been reported due to the ongoing pandemic [7]. The prevalence of mucormycosis is estimated to be around 70 times higher in India than globally, which were estimated to be at 0.02 to 9.5 cases (with a median of 0.2 cases) per 100,000 persons [5,6]. Patients with post-pulmonary tuberculosis and chronic kidney disease are the emerging risk factor for developing mucormycosis in this country [5].
In our case, HIV seropositive due to illicit use of intravenous drug abuse (heroin addiction) is risk factor associated with the development of Pulmonary Mucormycosis. Moreover, HIV infection favoured a misleading diagnosis of other opportunistic infection such as Tuberculosis, aspergillosis, etc.
The clinical presentations of mucormycosis are classified on the basis of anatomic localisation, such as rhino-orbital-cerebral (ROCM), pulmonary, gastrointestinal, cutaneous, renal, and disseminated mucormycosis [8]. The ROCM type is the most common form of the disease in India, followed by the pulmonary and cutaneous types [9]; however, the pulmonary mucormycosis is the most common clinical presentation in developed countries [10]. Rhizopus arrhizus is the most common cause of mucormycosis in India, other agents like Rhizopus microsporus, Rhizopus homothallicus, and Apophysomyces variabilis are rising6.
Pulmonary mucormycosis is the rapidly progressive infection that occur after inhalation of spores into respiratory tract or by hematogenous or lymphatic spread [11]. It may present with nonspecific symptoms like cough, dyspnoea, chest pain, and fever [11]. Most patients present with fever and haemoptysis which can be massive sometimes. Haemoptysis results from angioinvasion which results in infarction and necrosis of the tissue, can leads to cavitation and haemoptysis, if major vessel gets involved it may be fatal [12].
The diagnosis of mucormycosis is made by histopathology and direct microscopy along with culture of the respective clinical specimens [13]. On histopathological examination, mucormycosis species appear as broad, nonseptate hyphae with right angle branching. Patient suspected of Pulmonary mucormycosis should be differentiated from aspergillosis as on histopathological examination Aspergillus shows regular, septate hyphae with acute angle branching [14].
Radiologically, the appearance of pulmonary mucormycosis is non-specific. Chest radiograph is abnormal in > 80% of patients [15]. Most common radiographic finding include lobar and segmental consolidation, in some patients it can be multi-lobar in distribution. Other findings include ground-glass lesions generally progress to consolidation, multiple pulmonary nodule or masses which may have ground-glass halo (halo sign), which may progress to reverse halo sign with central necrosis, rarely cavity formation, and the air-crescent sign. As the fungus is angio-invasive, it causes the vascular findings like pulmonary artery pseudoaneurysms, and abrupt termination of pulmonary artery branch appearing as vascular cut-off sign. It can spread to pleura, chest wall and mediastinum causing lymphadenopathy, surgical emphysema and pleural thickening or effusion. Cavitation is seen in 40% of cases, but the air-crescent sign is rarely seen [16]. The presence of the air-crescent sign is an ominous sign, thus surgical management should not be delayed. High-resolution CT chest is used to determine the extent of disease with high sensitivity in Pulmonary mucormycosis.
In pulmonary mucormycosis, early diagnosis is important for the patient’s survival due to rapid clinical course of progression and angio-invasive nature of the disease. For the definitive diagnosis, hyphae of the fungus should be identified in the appropriate clinical specimen. The diagnostic techniques include percutaneous needle biopsy, open lung biopsy and pleural fluid culture. Fiberoptic bronchoscopy is a useful diagnostic method, and an adequate bronchoalveolar lavage specimen provides enough diagnostic material to form a cytological diagnosis [17]. Clinical presentation of Pulmonary mucormycosis is non-specific, thus it should be differentiated from other bacterial, viral and fungal pulmonary infections. Most importantly, Pulmonary mucormycosis should be differentiated from Invasive aspergillosis so that appropriate treatment should be given for patient’s survival [16].
Treatment of pulmonary mucormycosis include medical treatment with the recommended antifungal therapy and extensive surgical debridement [18]. Surgical resection of the infected parenchyma should be considered an early intervention to improve survival, due to the limited penetration of anti-fungal to the affected necrotic tissues, that accompanies this infection. The recommended antifungal agent is liposomal amphotericin B, subsequently, posaconazole and isavuconazole are prescribed [19].
The major drawbacks in managing mucormycosis in India are a gap in treatment protocol and the financial constraints of patients that they cannot afford liposomal amphotericin B. Pulmonary Mucormycosis is a relatively uncommon disease in comparison with Pulmonary Tuberculosis which is highly prevalent disease in India especially in patient living with HIV infection (PLHIV). Another drawback is over-reliance in chest radiograph for diagnosis of Pulmonary Tuberculosis. A high level of clinical suspicion in patients with post-pulmonary tuberculosis is important, in the presence of appropriate clinical setting and a non-resolving pulmonary opacity with cavitation for considering invasive fungal infection as differential diagnosis in immunocompromised patients.
Mucormycosis is an opportunistic life-threatening infection mostly occurring in the immunocompromised host. Pulmonary mucormycosis should be suspected in immunocompromised patient like HIV infection and patients with post-pulmonary tuberculosis in country like India, particularly when they present with non-resolving pulmonary opacification with cavitation despite being on anti-tubercular therapy and when patient was already been treated with anti-tubercular therapy for Pulmonary tuberculosis. High clinical suspicion is required for early diagnosis of patient. Early diagnosis and treatment of patient with surgical debridement and medical treatment with recommended antifungal drugs can improve outcome and survival in Pulmonary mucormycosis.
- Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000; 13: 236–301. PubMed: https://pubmed.ncbi.nlm.nih.gov/10756000/
- Hibbett DS, Binder M, Bischoff JF, Blackwell M, Cannon PF, et al. A higher‑level phylogenetic classification of the Fungi. Mycol Res. 2007; 111: 509-547. PubMed: https://pubmed.ncbi.nlm.nih.gov/17572334/
- Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: Pathophysiology, presentation and management. Clin Microbiol Rev. 2005; 18: 556-569. PubMed: https://pubmed.ncbi.nlm.nih.gov/16020690/
- Fürbringer P. Observations on pulmonary mucormycosis in humans. Virchows Arch Path Anat. 1976; 66: 330-365.
- Prakash H, Chakrabarti A. Epidemiology of Mucormycosis in India. Microorganisms. 2021; 9: 523. PubMed: https://pubmed.ncbi.nlm.nih.gov/33806386/
- Prakash H, Chakrabarti A. Global Epidemiology of Mucormycosis. J Fungi (Basel). 2019; 5: 26. PubMed: https://pubmed.ncbi.nlm.nih.gov/30901907/
- Garg D, Muthu V, Sehgal IS, Ramachandran R, Kaur H, et al. Coronavirus Disease (Covid-19) Associated Mucormycosis (CAM): Case Report and Systematic Review of Literature. Mycopathologia. 2021; 186: 289-298. PubMed: https://pubmed.ncbi.nlm.nih.gov/33544266/
- Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, et al. The epidemiology and clinical manifestations of mucormycosis: A systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019; 25: 26–34. PubMed: https://pubmed.ncbi.nlm.nih.gov/30036666/
- Prakash H, Ghosh AK, Rudramurthy SM, Singh P, Xess I, et al. A prospective multicenter study on mucormycosis in India: Epidemiology, diagnosis, and treatment. Med Mycol. 2019; 57: 395–402. PubMed: https://pubmed.ncbi.nlm.nih.gov/30085158/
- Skiada A, Pagano L, Groll A, Zimmerli S, Dupont B, et al. Zygomycosis in Europe: Analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) Working Group on Zygomycosis between 2005 and 2007. Clin Microbiol Infect. 2011; 17: 1859–1867. PubMed: https://pubmed.ncbi.nlm.nih.gov/21199154/
- Serris F. Danion F, Lanternier F. Disease entities in mucormycosis. J Fungi. 2019; 5: 23. PubMed: https://pubmed.ncbi.nlm.nih.gov/30875744/
- Garg R, Marak RS, Verma SK, Singh J, Sanjay, et al. Pulmonary mucormycosis mimicking as pulmonary tuberculosis: a case report. Lung India. 2008; 25: 129–131. PubMed: https://pubmed.ncbi.nlm.nih.gov/20165666/
- Challa S, Uppin SG, Uppin MS, Paul RT, Prayaga AK, et al. Pulmonary zygomycosis: a clinicopathological study. Lung India. 2011; 28: 25–29. PubMed: https://pubmed.ncbi.nlm.nih.gov/21654982/
- Song JG, Kang SH, Jung BW, Oh HS, Kim MJ, et al. Invasive pulmonary aspergillosis histologically mimicking mucormycosis. The Ewha Med J. 2016; 39: 65–68.
- Donado‑Uña JR, Díaz‑Hellín V, López‑Encuentra A, Echave-Sustaeta JM. Persistent cavitations in pulmonary mucormycosis after apparently successful amphotericin B. Eur J Cardiothorac Surg. 2002; 21: 940-942. PubMed: https://pubmed.ncbi.nlm.nih.gov/12062298/
- Chung JH, Godwin JD, Chien JW, Pipavath SJ. Case 160: Pulmonary mucormycosis. Radiology. 2010; 256: 667-670. PubMed: https://pubmed.ncbi.nlm.nih.gov/20656848/
- Al‑Abbadi MA, Russo K, Wilkinson EJ. Pulmonary mucormycosis diagnosed by bronchoalveolar lavage: A case report and review of the literature. Pediatr Pulmonol. 1997; 23: 222-225. PubMed: https://pubmed.ncbi.nlm.nih.gov/9094732/
- Tedder M, Spratt JA, Anstadt MP, Hegde SS, Tedder SD, et al. Pulmonary mucormycosis: results of medical and surgical therapy. Ann Thorac Surg. 1994; 57: 1044–1050. PubMed: https://pubmed.ncbi.nlm.nih.gov/8166512/
- Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, et al. Global guideline for the diagnosis and management of mucormycosis: An initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019; 19: e405–e421. PubMed: https://pubmed.ncbi.nlm.nih.gov/31699664/